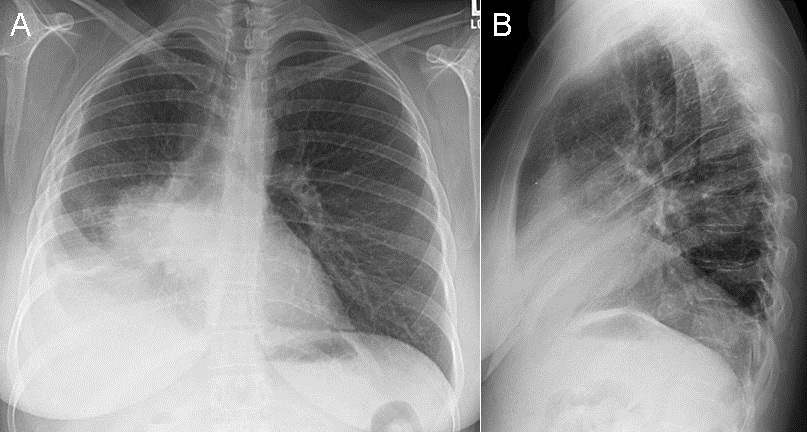
Figure 1. Left subclavian central line courses in a left paramediastinal location.
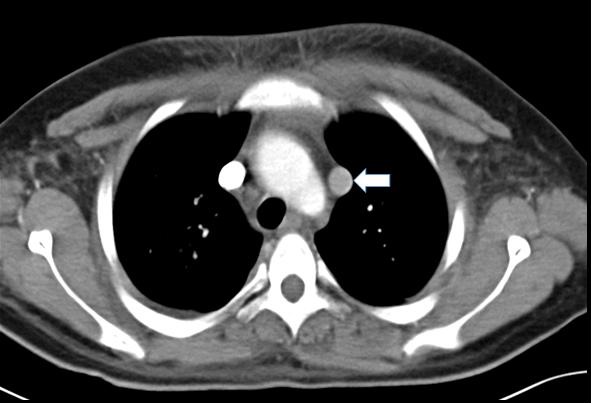
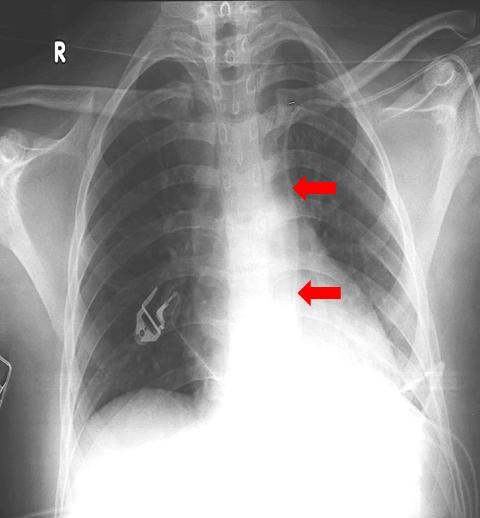
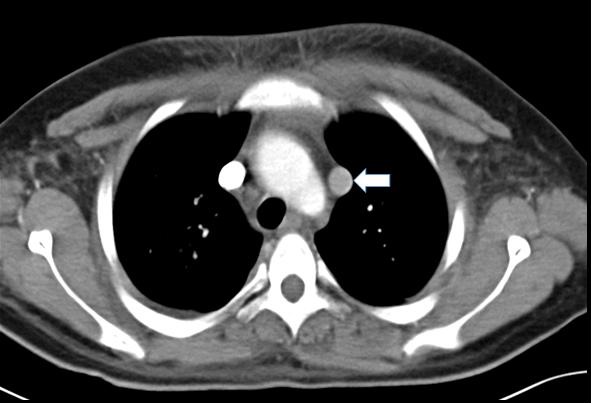
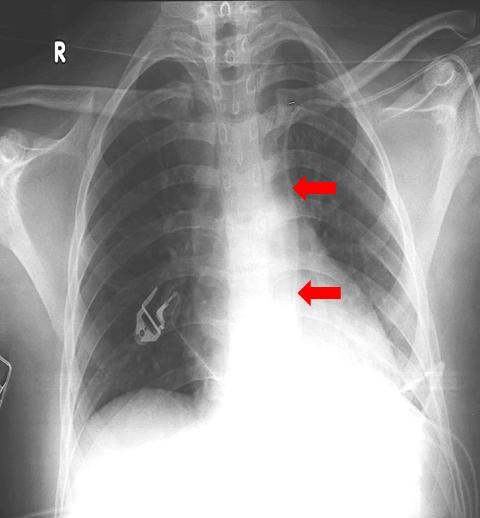
Figure 2. Axial CT image of the chest shows a vessel coursing lateral to the aortic arch consistent with a persistent left superior vena cava.
A 19 year old man with acute lymphocytic leukemia was admitted to the ICU with septic shock. Due to areas of cellulitis on the right side of the chest and neck and femoral venous thrombi, a left subclavian central access was attempted. The chest x-ray obtained after line placement is shown below (Figure 1). Blood gas done from the line was consistent with venous blood and venous tranduction was seen. A CT of the chest (Figure 2) confirmed the diagnosis of persistent left superior vena cava (PLSVC).
A persistent left superior vena cava is the most common congenital thoracic venous anomaly, seen in 0.3-0.5% of the population (1). Incidence is increased in patients with congenital heart disease to 5%. In most patients a right sided SVC is also present; hence the term SVC duplication has also been used. Embryologically a PLSVC is formed when the left anterior cardinal vein is not obliterated during fetal development to form the ‘Ligament of Marshall’. It usually drains in to the coronary sinus.
Diagnosis is usually made incidentally on CT scan, echocardiography or,like in our case, after a left sided central access. Practically, its presence may complicate left sided central access including Swan Ganz Catheter placement, implantable cardioverter defibrillator (ICD) placement and during cardiac surgery including during administration of retrograde cardioplegia or cardiac transplant.
Emad Hammode MD1, Khaled Hamed MD1, Mohammad Hudeeb MD1, Veronica Arteaga MD2
1Department of Internal Medicine
2Department of Thoracic Imaging
University of Arizona Medical Canter
Tucson, AZ
Reference
- Povoski SP, Khabiri H. Persistent left superior vena cava: review of the literature, clinical implications, and relevance of alterations in thoracic central venous anatomy as pertaining to the general principles of central venous access device placement and venography in cancer patients. World J Surg Oncol. 2011;9:173. [CrossRef] [PubMed]
Reference as: Hammode E, Hamed K, Hudeeb M, Arteaga V. Medical image of the week: persistent left superior vena cava. Southwest J Pulm Crit Care. 2014;9(4):242-3. doi: http://dx.doi.org/10.13175/swjpcc132-14 PDF
 Monday, November 3, 2014 at 8:00AM
Monday, November 3, 2014 at 8:00AM