Medical Image of the Month: Buffalo Chest Identified at the Time of Lung Nodule Biopsy
 Monday, November 2, 2020 at 8:00AM
Monday, November 2, 2020 at 8:00AM 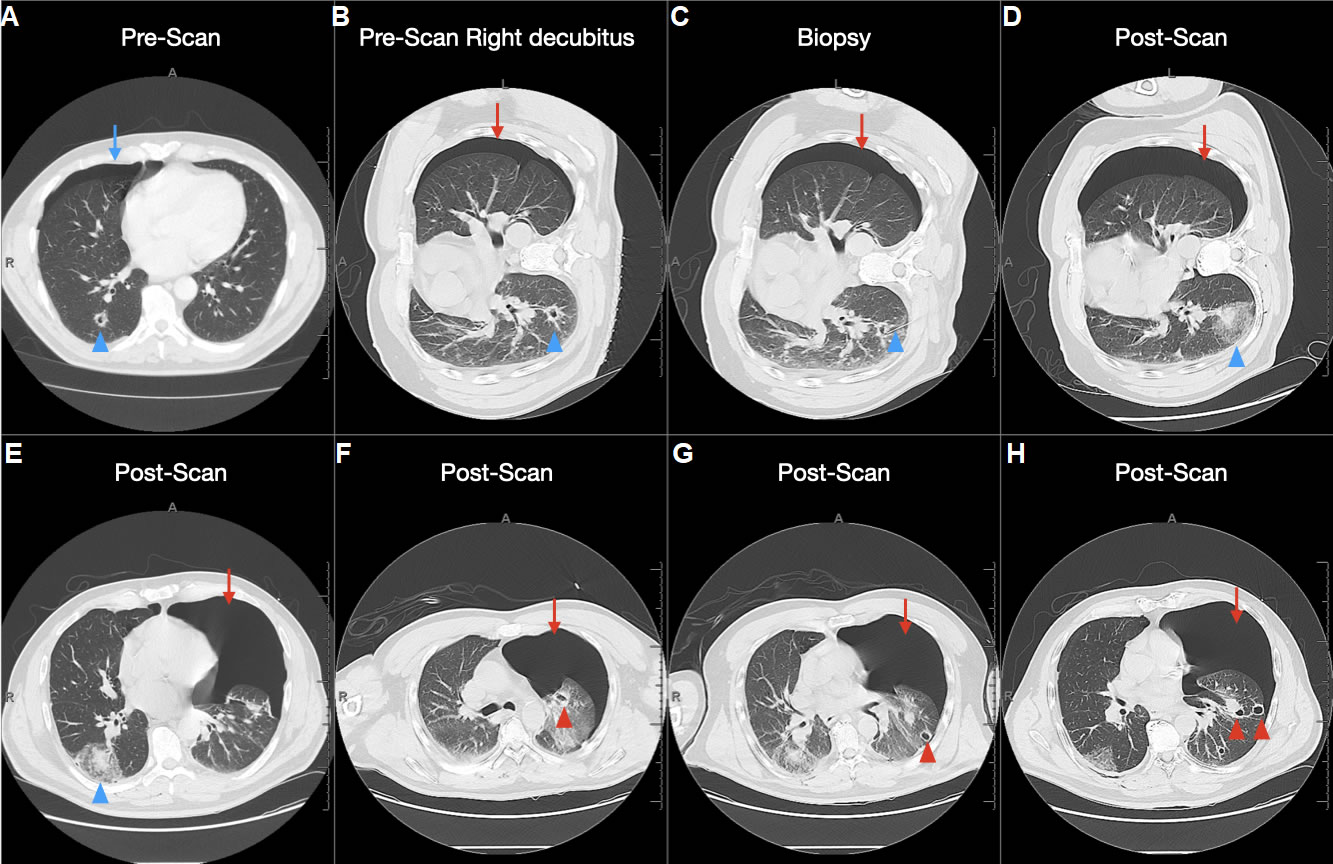
Figure 1. Buffalo chest, peripheral cavitary lesions, and pneumothorax contralateral to the biopsy site. A) Outpatient CT scan showing a right pneumothorax (blue arrow) and right-sided cavitary lesion (blue arrowhead). B) Subsequent pre-procedural planning CT scan done right lateral decubitus, showing again the cavitary lesion (blue arrowhead) but now with left pneumothorax (red arrow), suggesting buffalo chest. C) Intra-procedural CT showing needle at the periphery of the cavitary lesion (blue arrowhead) and similar-sized left pneumothorax (red arrow). D) 5-minute post-procedural CT demonstrating expected alveolar hemorrhage in the site of the biopsied cavitary lesion (blue arrowhead), but worsening left pneumothorax (red arrow). E & F) Multiple peripheral left lung cavitary lesions (red arrowheads) felt to be possible culprits for the worsened pneumothorax following coughing from the right-sided biopsy.
A gentleman in his late 50s with a past medical history of squamous cell carcinoma at the base of the tongue had numerous slowly-growing pneumocyst-like lesions despite clinical remission status post surgery and chemoradiation. Biopsy of one of these lesions was recommended by a multidisciplinary tumor board.
An outpatient pre-procedural supine chest CT revealed a right pneumothorax above the lesion targeted for biopsy. A subsequent pre-procedural right lateral decubitus chest CT three weeks later demonstrated a left-sided pneumothorax, raising concern for buffalo chest. (A less likely possibility would be spontaneous resolution of the right pneumothorax and development of a new left pneumothorax in the less than 4-week interval.) Intraprocedural imaging continued to demonstrate the left-sided pneumothorax. A biopsy touch preparation of the first sample obtained did not demonstrate malignancy. Therefore, an attempt was made at obtaining another sample. However, the patient developed a brief but forceful coughing fit, resulting in the termination of the procedure after only 2 passes of a 20g needle. Post-procedural scans demonstrated expected right-sided alveolar hemorrhage near the biopsy tract but slight worsening of the contralateral pneumothorax. The patient was again scanned five minutes later for concerns of a worsening pneumothorax. CT imaging demonstrated stable right-sided alveolar hemorrhage near the biopsy tract, but also severe left sided pneumothorax with multiple peripheral cavitary lesions. A left anterior chest tube was placed and the patient was discharged a few days later. Biopsy results showed granulomatous tissue only and cultures were negative.
Buffalo chest refers to the abnormal presence of a pleuro-pleural communication in humans. This phenomenon derives its name from the fact that buffalo and similar species possess one contiguous pleural space, while humans ordinarily have two independent pleural spaces corresponding to each lung (1). This pleuro-pleural communication can develop iatrogenically, congenitally, or as a result of trauma. Cases of buffalo chest developing after median sternotomy, laparoscopic surgery and heart-lung transplantation have been described in the literature (2). It is unknown if the worsening of our patient’s left-sided pneumothorax occurred in the setting of underlying buffalo chest, with biopsy producing a right sided pneumothorax that subsequently communicated with the left pleural space. Alternatively, our patient’s episode of forceful coughing could have increased the intrathoracic pressure and caused barotrauma to one of the many peripheral cavitary lesions previously described, leading to a worsening of the left-sided pneumothorax. Cases of bilateral pneumothoraces where interpleural connections exist have been successfully treated with a unilateral chest tube (2, 3). A second chest tube may be necessary in cases where the contralateral lung fails to re-expand. Our patient was able to be discharged after placement of a unilateral chest tube (contralateral to the biopsy side), reaffirming the general recommendation to treat pneumothoraces this patient population with a unilateral pleural catheter.
Phillip Belone MS4, Jason Lee MD, and Michael Craig Larson MD PhD
University of Arizona/Banner University Medical Center-Tucson
Department of Medical Imaging
Tucson, AZ USA
References
- Jacobi A, Eber C, Weinberger A, Friedman SN. Bilateral Pneumothoraces after Unilateral Lung Biopsy. A Case of "Buffalo Chest"? Am J Respir Crit Care Med. 2016 Apr 15;193(8):e36. [CrossRef] [PubMed]
- Sawalha L, Gibbons WJ. Iatrogenic "buffalo chest" bilateral pneumothoraces following unilateral transbronchial lung biopsies in a bilateral lung transplant recipient. Respir Med Case Rep. 2015 May 16;15:57-8. [CrossRef] [PubMed]
- Groarke J, Breen D, O'Connell F, O'Donnell R. Bilateral pneumothorax resulting from a diagnostic thoracentesis. Eur Respir J. 2007 Nov;30(5):1018-9; diagnosis 1020. [CrossRef] [PubMed]
Cite as: Belone P, Lee J, Larson MC. Medical Image of the Month: Buffalo Chest Identified at the Time of Lung Nodule Biopsy. Southwest J Pulm Crit Care. 2020;21(5):121-3. doi: https://doi.org/10.13175/swjpcc056-20 PDF

Reader Comments