Medical Image of the Month: Severe Acute Respiratory Distress Syndrome and Embolic Strokes from Polymethylmethacrylate (PMMA) Embolization
 Friday, April 2, 2021 at 8:00AM
Friday, April 2, 2021 at 8:00AM 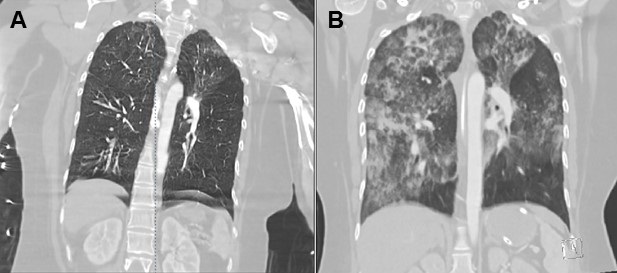
Figure 1. The contrast-enhanced CT of the chest on the left (Panel A) was acquired at the time of admission. The contrast-enhanced CT of the chest on the right (Panel B) was obtained 3 days into the hospitalization. The initial study demonstrated ground glass opacities most pronounced in the upper lobes, left greater than right. The follow up CT demonstrated marked progression of her airspace disease bilaterally, consistent with the clinical picture of the adult respiratory distress syndrome (ARDS).
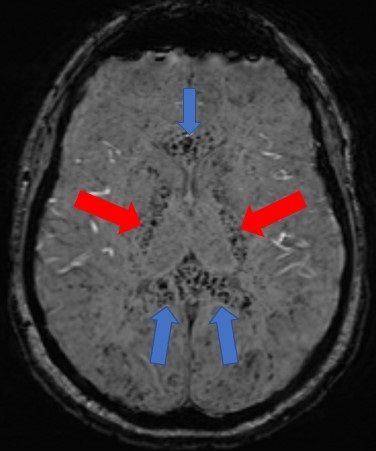
Figure 2. An axial susceptibility weighted image (SWI) of the brain demonstrates extensive foci of susceptibility artifact (black dots) most pronounced in the genu and splenium of the corpus callosum (blue arrows) and the bilateral internal capsules (red arrows) – most consistent with embolic phenomenon.
A 35-year-old lady with a history of depression and anxiety presented to the emergency room with worsening shortness of breath after receiving polymethylmethacrylate (PMMA) injections in her buttock for cosmetic purposes in Mexico. Immediately after the injection in the outpatient office, she became acutely short of breath, tachypneic, and tachycardic. She was brought to the emergency room where she was hypoxic with oxygen saturations in the low 80s on a non-rebreather, tachypneic with a respiratory rate in the 40s, and tachycardic with heart rates in 140s. She was emergently intubated. A CTA of the chest demonstrated bilateral ground glass opacities throughout, most pronounced in the upper lobes which progressed to significant bilateral airspace disease consistent with acute respiratory distress syndrome (Figure 1). Her neurological examination declined over the course of her hospitalization. An MRI of the brain with contrast demonstrated bilateral foci of susceptibility artifact throughout the entirety of the brain most consistent with an embolic phenomenon in the setting of a suspected right-to-left shunt (Figure 2). Her mental status did not improve during her hospital course, and her family was deciding on whether to pursue comfort measures.
Discussion: Embolic complications of PMMA have been documented in the literature in relation to interventional procedures of the spine where it is used as a cement (i.e. vertebroplasty/kyphoplasty) (1). In those instances, the emboli are radiopaque and can be identified on conventional imaging modalities such as chest radiography or CT imaging (2). In the case of our patient, we were not able to confirm the exact formulation of the PMMA, but we suspect that it was delivered in the form of a dermal filler which was likely in the form of particles/microspheres. Migration of the particles/microspheres in the form of vascular emboli can occur if injected into blood vessels during procedures (3).
Sooraj Kumar MBBS1, Sharanyah Srinivasan MBBS1, and Tammer El-Aini MD2
1Banner University Medical Center – South Campus, Department of Internal Medicine
2Banner University Medical Center – Main Campus, Department of Pulmonary and Critical Care
References
- Abdul-Jalil Y, Bartels J, Alberti O, Becker R. Delayed presentation of pulmonary polymethylmethacrylate emboli after percutaneous vertebroplasty. Spine (Phila Pa 1976). 2007 Sep 15;32(20):E589-93. [CrossRef] [PubMed]
- Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br. 2003 Jan;85(1):83-9. [CrossRef] [PubMed]
- Lemperle G, Morhenn VB, Pestonjamasp V, Gallo RL. Migration studies and histology of injectable microspheres of different sizes in mice. Plast Reconstr Surg. 2004 Apr 15;113(5):1380-90. [CrossRef] [PubMed]
Cite as: Kumar S, Srinivasan S, El-Aini T. Medical image of the month: severe acute respiratory distress syndrome and embolic strokes from polymethylmethacrylate (PMMA) embolization. Southwest J Pulm Crit Care. 2021;22(4):86-7. doi: https://doi.org/10.13175/swjpcc008-21 PDF

Reader Comments