April 2024 Medical Image of the Month: Wind Instruments Player Exhibiting Exceptional Pulmonary Function
 Tuesday, April 2, 2024 at 8:00AM
Tuesday, April 2, 2024 at 8:00AM  Figure 1. Representative view from computed tomography (CT) scan (axial plane) showing clear lungs.
Figure 1. Representative view from computed tomography (CT) scan (axial plane) showing clear lungs.
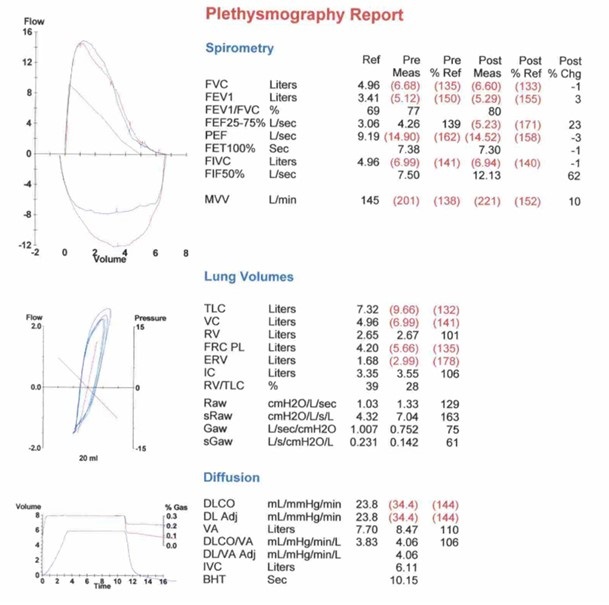 Figure 2. Pulmonary function testing results demonstrating exceptional pulmonary function
Figure 2. Pulmonary function testing results demonstrating exceptional pulmonary function
A 64-year-old man was referred to our pulmonary clinic for evaluation of his pulmonary status. He had a 7-year history of rheumatoid arthritis and was treated initially with steroids and subsequently maintained on methotrexate and monthly adalimumab injections. The patient reported that his rheumatoid arthritis symptoms were controlled. He experienced no joint pain or morning stiffness at the time of evaluation. From a pulmonary perspective, he denied respiratory symptoms such as exertional shortness of breath, cough, wheezing, or chest tightness. He reported no limitations in physical activities. The patient has an occupational history of 45-years as a welder, with exposure to dust, metal fumes, benzene, and sulfur gas. The patient also has a 15 pack-year smoking history but quit 35 years ago.
A high-resolution chest CT (Figure 1) ordered by his rheumatologist showed normal lung parenchyma. The first pulmonary function test (PFT), conducted on the initial pulmonary clinic visit, revealed lung volumes significantly higher than the reference range. This is despite the patient’s occupational history, smoking history, and the fact that he is currently on methotrexate and adalimumab therapy. The patient remained asymptomatic from a pulmonary standpoint on annual checkups. Three years later, a repeat PFT (Figure-2) demonstrated similar results. Further history revealed that the patient had regularly used wind instruments, including the saxophone and harmonica, since high school. Initially, he played at irregular intervals, but for the last 15 years, he consistently practiced 1-2 hours daily and performed weekly at local venues.
Several studies have investigated the pulmonary effects of wind instrument playing, offering insights into the relationship between musical activities and respiratory function. Fiz et al. (1) found that maximum respiratory pressures were elevated in trumpet players. Munn et al. (2) reported on the pulmonary function of commercial glass blowers [2]. Barbenel et al. (3) explored mouthpiece forces during trumpet playing and Kahane et al. (4) evaluated the upper airway and larynx in professional bassoon players. Cossette et al. (5) examined chest wall dynamics during flute playing. Schorr-Lesnick et al. (6) studied pulmonary function in singers and wind-instrument players [6], and Navratil et al. (7) assessed lung function in wind instrument players and glass blowers. Borgia et al. (8) provided physiological observations on French horn musicians. While existing studies present conflicting findings on the impact of wind instrument playing on respiratory function, our case adds to the growing body of evidence suggesting a potential positive correlation between long-term wind instrument training and enhanced respiratory muscle strength.
This observation prompts further exploration and investigation into the field of pulmonary rehabilitation with the hope of uncovering therapeutic benefits for individuals with chronic pulmonary conditions.
Abdulmonam Ali, MD
Pulmonary & Critical Care
SSM Health
Danville, IL USA
References
- Fiz JA, Aguilar J, Carreras A, Teixido A, Haro M, Rodenstein DO, Morera J. Maximum respiratory pressures in trumpet players. Chest. 1993 Oct;104(4):1203-4. [CrossRef] [PubMed]
- Munn NJ, Thomas SW, DeMesquita S. Pulmonary function in commercial glass blowers. Chest. 1990 Oct;98(4):871-4. [CrossRef] [PubMed]
- Barbenel JC, Kenny P, Davies JB. Mouthpiece forces produced while playing the trumpet. J Biomech. 1988;21(5):417-24. [CrossRef] [PubMed]
- Kahane JC, Beckford NS, Chorna LB, Teachey JC, McClelland DK. Videofluoroscopic and laryngoscopic evaluation of the upper airway and larynx of professional bassoon players. J Voice. 2006 Jun;20(2):297-307. [CrossRef] [PubMed]
- Cossette I, Monaco P, Aliverti A, Macklem PT. Chest wall dynamics and muscle recruitment during professional flute playing. Respir Physiol Neurobiol. 2008 Feb 1;160(2):187-95. [CrossRef] [PubMed]
- Schorr-Lesnick B, Teirstein AS, Brown LK, Miller A. Pulmonary function in singers and wind-instrument players. Chest. 1985 Aug;88(2):201-5. [CrossRef] [PubMed]
- Navratil M, Bejsek K. Lung function in wind instrument players and glass blowers. Ann NY Acad Sci. 1968; 155:276-83.
- Borgia JF, Horvath SM, Dunn FR, von Phul PV, Nizet PM. Some physiological observations on French horn musicians. J Occup Med. 1975 Nov;17(11):696-701. [PubMed]

Reader Comments