September 2022 Medical Image of the Month: Epiglottic Calcification
 Friday, September 2, 2022 at 8:00AM
Friday, September 2, 2022 at 8:00AM 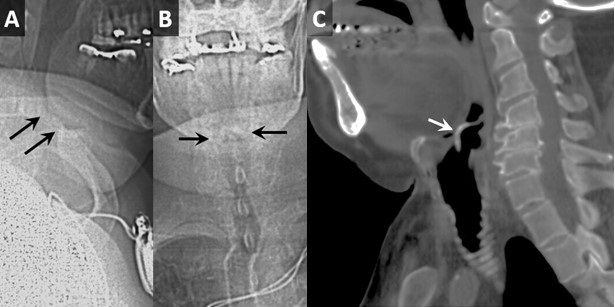 Figure 1. Lateral (A) and frontal (B) topogram from a neck CT demonstrates linear calcifications in the expected location of the epiglottis (black arrows). Sagittal multiplanar reconstructions demonstrate prominent calcification of the epiglottis (white arrow).
Figure 1. Lateral (A) and frontal (B) topogram from a neck CT demonstrates linear calcifications in the expected location of the epiglottis (black arrows). Sagittal multiplanar reconstructions demonstrate prominent calcification of the epiglottis (white arrow).
In consideration of dysphagia, most cases predominate in the oropharyngeal region with the remainder caused primary by esophageal causes. Lesser known and studied is the development of dysphagia and globus sensation from epiglottic pathology, namely epiglottic calcification. With less than a dozen published cases in literature, very little data exists on identification, diagnosis, and treatment of this known cause of morbidity. Here we present a case of oropharyngeal dysphagia arising from a rare cause, epiglottic calcification.
An 81-year-old man with a history of aortic stenosis and carotid artery stenosis presented with worsening dysphagia over the course of one month. The patient reported significant dysphagia, initially to solids and subsequently to liquids causing a weight loss of over 50 pounds. Physical exam of the oropharynx and neck were unremarkable. A bedside swallow evaluation suggested mildly decreased hyolaryngeal movement, but no other significant abnormalities. A barium swallow study revealed incomplete epiglottic excursion during the pharyngeal phase of swallowing. The patient then underwent evaluation with a contrast-enhanced esophagogram, which showed severe esophageal dysmotility and gastroesophageal reflux. A CT of the neck demonstrated calcification of the epiglottis without epiglottal enlargement. ENT was consulted, the patient underwent flexible fiberoptic laryngoscopy and also EGD with biopsy. No other esophageal or gastric pathology were identified other than the epiglottic calcification. As no effective treatment is known at this time, the patient was changed to a modified diet with ongoing speech and swallow therapy as an outpatient.
Epiglottic calcification is a rare cause of dysphagia that is poorly understood in its etiology, clinical course and outcome (1). This case demonstrates that despite consultant team recommendations, no clear evaluation pathway or treatment currently exists. Currently, diagnosis can be accomplished with radiologic evaluation along with exclusion of other causes; however, no definitive treatments are available for this rare condition. Although the condition itself is rare, epiglottic calcification should be considered when other more common causes of significant dysphagia are ruled out.
Shil Punatar DO1, Dayoung Song MD1, Azkaa Zaman DO1, Benjamin Jiao DO2, and Tilemahos Spyratos DO1,3
1Department of Internal Medicine, Franciscan Health, Olympia Fields, IL
2Department of Radiology, Franciscan Health, Olympia Fields, IL
3Department of Gastroenterology, Franciscan Health, Olympia Fields, IL
Reference
1. Günbey HP, Günbey E, Sayit AT. A rare cause of abnormal epiglottic mobility and dyspagia: calcification of the epiglottis. J Craniofac Surg. 2014 Nov;25(6):e519-21. [CrossRef[[PubMed]

Reader Comments (1)
Epiglottic Calcification: The Unexplored Relationship with Increasing Rates of Renal Disease
To the Editor: In the September 2022 issue the Southwest Journal of Pulmonary Critical Care and Sleep published an interesting article authored by Punatar et al. detailing a case of severe dysphagia that was secondary to isolated epiglottic calcifications seen on computed tomography and flexible fiberoptic laryngoscopy (1). The epiglottis plays a critical role in the prevention of aspiration and coordination of swallowing. Calcifications can severely alter its flexibility and limit oral intake. Isolated calcifications of the epiglottis and sequential dysphagia is not a common entity. With the increasing rates of chronic and end-stage renal disease, this letter is focused on increasing the awareness of extra-osseous manifestations of secondary hyperparathyroidism.
Secondary hyperparathyroidism is characterized by adaptive parathyroid gland hyperplasia to increase the production of parathyroid hormone. Etiologies include vitamin D deficiency and chronic kidney disease. Vitamin D deficiency can be seen in about 50% of the world population and chronic kidney disease affects more than 37 million people in the United States (2-3). Manifestations of sustained increases in parathyroid hormone can cause high-turnover rates of osseous structures and extra-osseous manifestations. Among the extra-osseous manifestations, chondrocalcinosis is a known complication. Although there remains a higher risk of calcification within the larynx and trachea as opposed to the epiglottis, epiglottic calcifications should still be suspected in patients with dysphagia and chronic kidney disease (4-5). Early diagnosis and management may result in the prevention of worsening extra-osseous disease.
Given the lack of literature regarding the prevalence and characteristics of secondary hyperparathyroidism and epiglottic calcifications, all cases that identify epiglottic calcifications should note whether a secondary hyperparathyroidism work up or other causes of abnormal parathyroid hormone elevations was initiated, to aid the scientific community in identifying a potentially underdiagnosed phenomenon. My question to the authors of this study is if any further work up was completed, including biochemical serum testing for parathyroid hormone, vitamin D levels, calcium, or phosphate levels. This would be valuable for the audience of this journal and would allow providers to be increasingly aware of this clinical entity.
Ramzi Ibrahim MD
Department of Medicine – University of Arizona Tucson, Tucson, AZ USA
References
1. Punatar S, Song D, Zaman A, Jiao B, Spyratos T. September 2022 Medical Image of t
he Month: Epiglottic Calcification. Southwest J Pulm Crit Care Sleep. 2022;25(3):41-42.
2. Bouillon R, Norman AW, Lips P. Vitamin D deficiency. N Engl J Med. 2007 Nov 8;357(19):1980-1; author reply 1981-2.
3. Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2021. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021.
4. Ajmani ML, Jain SP, Saxena SK. A metrical study of laryngeal cartilages and their ossification. Anat Anz. 1980;148(1):42-8.
5. Fernández-Rodríguez A, Benito-Orejas JI, Jiménez-Pérez AE, Morais-Pérez D. Calcificación de la epiglotis [Calcification of the epiglottis]. Acta Otorrinolaringol Esp. 2009 May-Jun;60(3):215-6. Spanish.
The Author Replies: Dr. Ibrahim reflects on our contribution of a case of severe dysphagia secondary to epiglottic calcification. It is purported that cases of epiglottic calcification are not common, and that a workup for secondary hyperparathyroidism should be considered. This is suggested as secondary hyperparathyroidism from chronic kidney disease may cause extra-osseous manifestations such as calcifications of the larynx and trachea, and even epiglottis.
To confirm and collectively create a comprehensive understanding of our case of epiglottic calcification, we agree with the notion by Dr. Ibrahim that secondary hyperparathyroidism should be considered in causes of epiglottic calcification.
Upon further review with lab values included below, our patient had progressed from chronic kidney disease to end stage renal disease and was consistent with home peritoneal dialysis. It had been noted that the patient was undergoing care and monitoring for secondary hyperparathyroidism in the outpatient setting from nephrology services. While he was on calcitriol .5mcg daily in the outpatient, setting, we have included his pertinent lab values as follows:
• Calcium 9.3 mg/Dl( 8.6-10.3 mg/Dl)
• Corrected Calcium 10.1 mg/dL
• Albumin 3.0 g/dL (3.5-5.7 g/Dl)
• Phosphorus 3.6 mg/dL (2.5-4.5mg/dL)
• Vitamin D 25 0H 37.5 ng/ML (30-100 ng/ml)
While controlled, it is possible that secondary hyperparathyroidism a contributory factor in leading to this patient’s epiglottic calcification and subsequent dysphagia.
Shil Punatar DO
Department of Internal Medicine- Franciscan Health Olympia Fields, Olympia Fields, Illinois USA
Cite as: Ibrahim R. Epiglottic Calcification: The Unexplored Relationship with Increasing Rates of Renal Disease. Southwest J Pulm Crit Care. 2022;25(4):50-51; author reply 51. doi: https://doi.org/10.13175/swjpccs043-22