Medical Image of the Month: Stercoral Colitis
 Thursday, September 2, 2021 at 8:00AM
Thursday, September 2, 2021 at 8:00AM 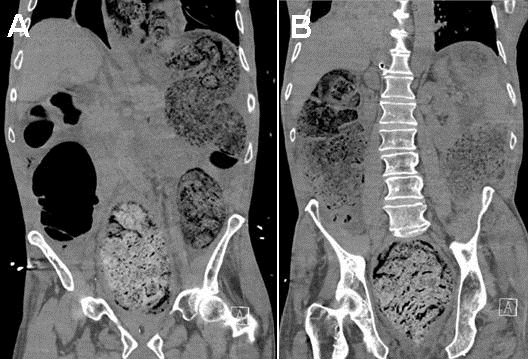
Figure 1. Non-contrast CT acquired at the time of admission demonstrating diffusely dilated large bowel loops from cecum to rectum measuring up to 8 cm. Image on the left (Panel A) shows a near-complete intrathoracic sliding-type herniation of stomach adjacent to a herniated portion of transverse colon through the diaphragm into the chest. The image on the right (Panel B) shows a markedly distended rectum with impacted stool with circumferential rectal wall thickening consistent with stercoral colitis.
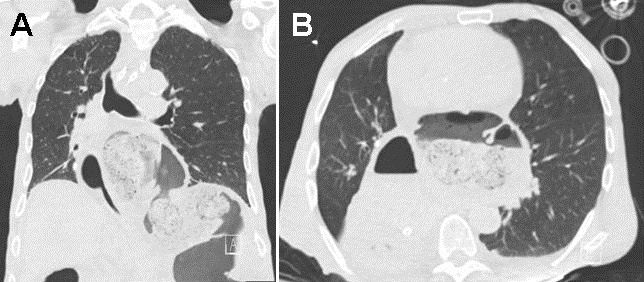
Figure 2. Non-contrast CT thorax demonstrating on the left (Panel A) large hiatal hernia with intrathoracic herniation of stomach and transverse colon. The image on the right (Panel B) shows mild mass effect upon the left atrium related to the herniated transverse colon.
A 78-year-old- man with cerebral palsy requiring an in-home caregiver presented to the emergency room in hypovolemic shock post-sudden cardiac arrest in the setting of hematemesis. The caregiver noticed the patient become unresponsive after having one episode of bright red emesis. EMS arrived and found the patient to be pulseless and performed three rounds of CPR and gave 1 mg of epinephrine before return of spontaneous circulation was obtained. The caregiver reported the patient had been complaining of diarrhea for the past few days after being started on magnesium citrate for constipation by his PCP. In the ED patient was intubated, sedated, and started on pressors due to undifferentiated shock. CT abdomen pelvis demonstrated diffuse dilation of the colon with massive stool burden and markedly distended rectum with impacted stool and circumferential rectal wall thickening consistent with stercoral colitis (Figures 1 and 2). In addition, there was a large hiatal hernia with intrathoracic herniation of the stomach and a portion of the transverse colon, but it did not appear to represent a point of high-grade obstruction. The patient was deemed a poor surgical or endoscopic candidate due to high perioperative mortality. Manual disimpaction was attempted with minimal stool output, mineral oil enemas were given, and OG tube decompression of stomach. The patient had a ST segment elevated myocardial infarction (STEMI) noted on EKG and despite pressors and aggressive IV fluid resuscitation patient’s condition continued to decline with family deciding to pursue comfort care. The patient’s profound constipation, large hiatal hernia, and stercoral colitis were contributing factors to his shock.
Stool impaction can occur secondary to chronic constipation as the colon absorbs salt and colitis is colonic perforation which has a mortality rate between 32-57 percent (1). The modality of choice for diagnosis is CT and the common findings are colonic wall thickening, pericolonic fat stranding, mucosal discontinuity, pericolonic abscess, and free air indicating perforation. A small retrospective study found that the most consistent findings in stercoral colitis were rectosigmoid colon involvement, dilation of the colon >6 cm, and bowel wall thickening >3 mm in the affected segment. It also suggests that colonic involvement of >40 cm and perforation indicate increased mortality (2,3). Stercoral colitis most commonly occurs in the elderly, those who are bedridden due to cerebrovascular events or severe dementia, chronic opioid use, malignancy, and those with motor disabilities, such as this patient with cerebral palsy. In patients without signs of peritonitis or who are poor surgical candidates can be managed non-operatively with laxatives, enemas, and manual/endoscopic disimpaction (4). Early diagnosis and treatment are imperative to avoid perforation. Patients with signs of perforation require surgical treatment which involves resection of the affected bowel segments.
Kirstin H. Peters MSIV, Angela Gibbs MD, Janet Campion MD
University of Arizona School of Medicine, Banner University Medical Center-Tucson, Tucson, AZ USA
References
- Serpell JW, Nicholls RJ. Stercoral perforation of the colon. Br J Surg. 1990 Dec;77(12):1325-9. [CrossRef] [PubMed]
- Ünal E, Onur MR, Balcı S, Görmez A, Akpınar E, Böge M. Stercoral colitis: diagnostic value of CT findings. Diagn Interv Radiol. 2017 Jan-Feb;23(1):5-9. [CrossRef] [PubMed]
- Wu CH, Wang LJ, Wong YC, et al. Necrotic stercoral colitis: importance of computed tomography findings. World J Gastroenterol. 2011 Jan 21;17(3):379-84. [CrossRef] [PubMed]
- Hudson J, Malik A. A fatal faecaloma stercoral colitis: a rare complication of chronic constipation. BMJ Case Rep. 2015 Sep 3;2015:bcr2015211732. [CrossRef] [PubMed]
Cite as: Peters KH, Gibbs A, Campion J. Medical Image of the Month: Stercoral Colitis. Southwest J Pulm Crit Care. 2021;23(3):73-5. doi: https://doi.org/10.13175/swjpcc027-21 PDF

Reader Comments