Medical Image of the Week: Metastatic Collecting Duct Carcinoma
 Wednesday, December 31, 2014 at 8:00AM
Wednesday, December 31, 2014 at 8:00AM C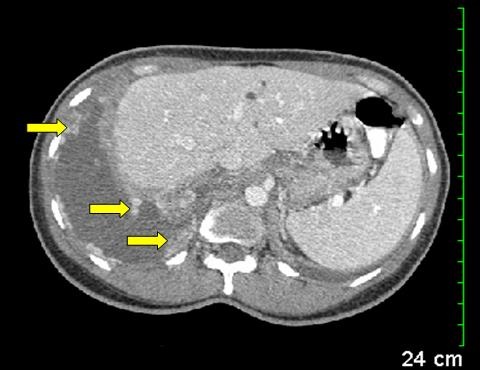
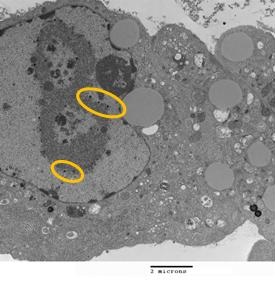
Figure 1. Transverse section of CT chest and abdomen shows enhancing pleural nodularity (yellow arrows) with a pleural effusion.

Figure 2. Transverse section of CT abdomen shows heterogeneous enhancing mass in the right kidney (red arrow).

Figure 3. Coronal section of CT chest and abdomen showing a large right pleural effusion (yellow arrow) and atelectatic lung with mediastinal shift to the left. Red arrow points to the heterogeneous mass in the right kidney.
A 40-year-old woman home health nurse presented to the ED with intermittent right sided sharp chest pain and progressive dyspnea for 2 weeks. On admission she was found to be in respiratory distress. Chest x-ray revealed a massive right sided pleural effusion. Thoracic CT scan with contrast confirmed a large right pleural effusion with associated enhancing pleural nodularity also involving the diaphragmatic surface (Figure 1). The visualized part of the abdomen revealed a mass in the midpole of right kidney (Figure 2). Subsequent CT scan of the abdomen with contrast revealed a heterogeneous enhancing mass in the right kidney suspicious for malignancy (Figure 3) and multiple paracaval lymph nodes. Thoracentesis revealed a hemorrhagic pleural effusion and during subsequent right video-assisted thoracoscopy showed disseminated tumorlets along the diaphragm and pleura. Pleural biopsy and fluid cytology was consistent with metastatic poorly differentiated collecting duct carcinoma of the kidney. The patient is currently getting outpatient chemotherapy. Collecting duct carcinoma of the kidney is an unusual variant of renal cell carcinoma and accounts for about 1% of all renal cell carcinomas (1). This variant has a poor prognosis and frequently metastasizes to the lung and liver.
Chandramohan Meenakshisundaram, MD
Nanditha Malakkla, MD
St. Francis Hospital.
Evanston, IL
Reference
- Wang X, Hao J, Zhou R, Zhang X, Yan T, Ding D, Shan L, Liu Z. Collecting duct carcinoma of the kidney: a clinicopathological study of five cases. Diagn Pathol. 2013;8:96. [CrossRef] [PubMed]
Reference as: Meenakshisundaram C, Malakkla N. Medical image of the week: metastatic collecting duct carcinoma. Southwest J Pulm Crit Care. 2014;9(6):348-9. doi: http://dx.doi.org/10.13175/swjpcc160-14 PDF