Medical Image of the Week: Coral Reef Aorta
 Wednesday, July 26, 2017 at 8:00AM
Wednesday, July 26, 2017 at 8:00AM 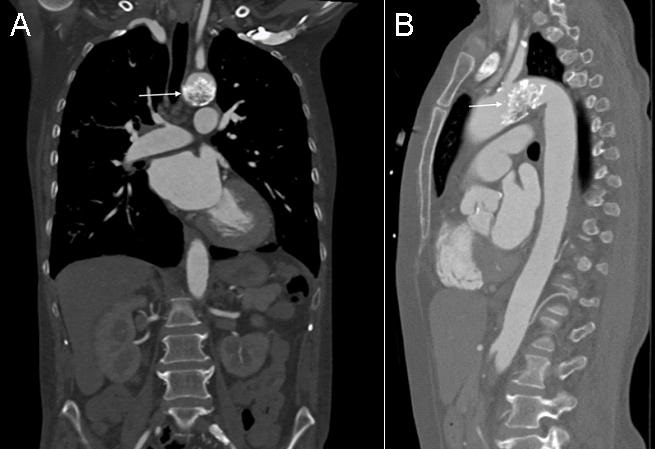
Figure 1. Coronal (A) and lateral (B) thoracic CT in soft tissue windows showing the coral reef calcification (arrows).
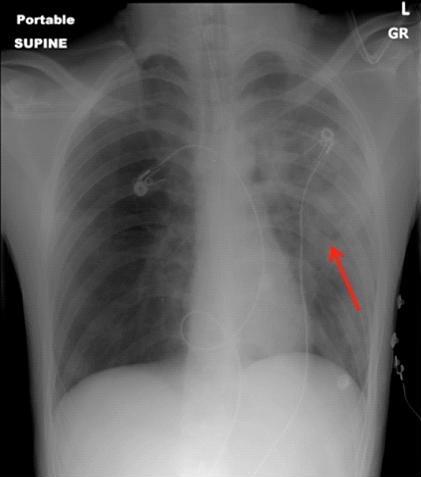
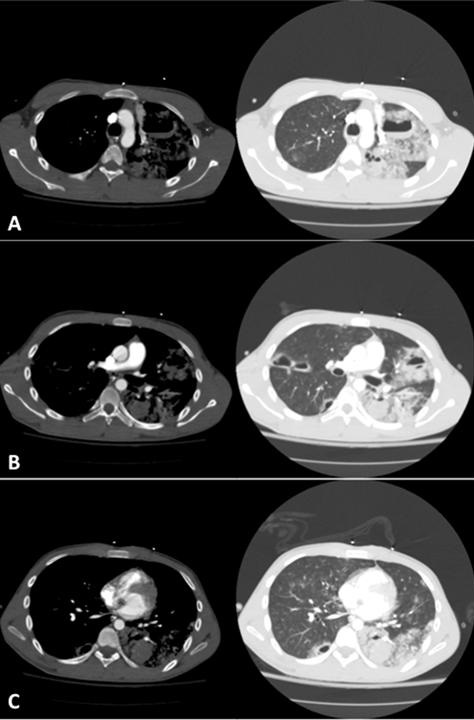
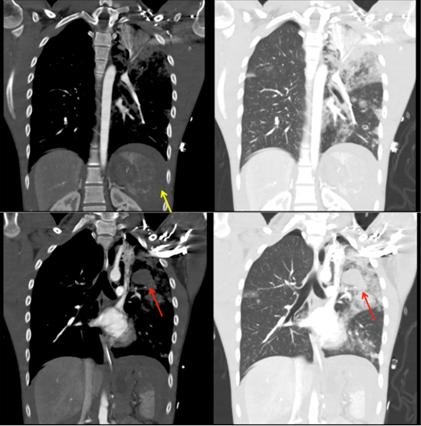
A 52-year-old woman with no past medical history presented to the emergency department with signs and symptoms concerning for pneumonia. Chest x-ray showed incidental findings of a calcified aortic mass. Subsequently, a follow up computed tomography scan (CT) was obtained which showed coral reef aorta (Figure 1). On physical examination, vital signs were only significant for mildly elevated blood pressure to 146/62 mmHg. She also had normal and equal pulses and pressures throughout all 4 extremities. In retrospect, patient had complaints of bilateral lower extremity claudication on strenuous exercise.
Coral reef aorta, a rare condition that was first described in 1984 by Qvarfordt et al. (1) is characterized by an eccentric, heavily calcified polypoid lesion and stenosis of the juxtarenal and suprarenal aorta. The rock-hard, irregular, gritty, whitish surface of the calcification strongly resembled a coral reef. The most common presentation is severe hypertension and intermittent claudication. Magnetic resonance angiogram (MRA) and CT have the ability to diagnose and appreciate the extent of this phenomenon (2).
Lance Eberson MS1 and Sehem Ghazala MD2
1College of Medicine and 2Department of Internal Medicine
University of Arizona
Tucson, Arizona, USA
References
- Qvarfordt PG, Reilly LM, Sedwitz MM, Ehrenfeld WK, Stoney RJ. "Coral reef" atherosclerosis of the suprarenal aorta: a unique clinical entity. J Vasc Surg. 1984 Nov;1(6):903-9. [CrossRef] [PubMed]
- Kopani K, Liao S, Shaffer K. The Coral Reef Aorta: Diagnosis and Treatment Following CT. Radiol Case Rep. 2016 Oct 4;4(1):209. eCollection 2009. [CrossRef] [PubMed]
Cite as: Eberson L, Ghazala S. Medical image of the week: coral reef aorta. Southwest J Pulm Crit Care. 2017:15(1):49. doi: https://doi.org/10.13175/swjpcc080-17 PDF