Ground-Glass Opacities
 Friday, June 3, 2011 at 4:04PM
Friday, June 3, 2011 at 4:04PM Reference as: Gopal V, Robbins RA. Ground-glass opacities. Southwest J Pulm Crit Care 2011;2:67-70. (Click here for PDF version)
A 54-year-old male was admitted to the medical intensive care unit complaining of abdominal pain, nausea, and vomiting for 2 days. He had a past medical history of pancreatitis in 2009, treated as outpatient, and asthma treated with albuterol inhaler as needed. His medication list included gemfibrizol, gabapentin, and amitriptyline. He drank 6-8 beers per day and smoked 1 pack-per-day for the past 40 years.
On physical examination is the patient was afebrile, his lungs are clear to auscultation, but tenderness was present in both lower quadrants. The remainder of the physical examination was normal.
Laboratory examination revealed a normal complete blood count and normal basic metabolic panel. Abnormal laboratory values included an elevated total bilirubin of 2.7 mg/dL (normal 0.2-1 mg/dL); alkaline phophatase 169 U/L (normal 10-40 U/L); alanine aminotransferase 286 U/L (normal 10-35 U/L); amylase 468 U/L (normal 25-125 U/L), and lipase 1580 U/L (normal 8-78 U/L). Arterial blood gasmeasurements showed PaO2 = 91 mm Hg, PaCO2 = 26 mm Hg, pH = 7.52, and oxygen saturation = 98% while breathing room air.
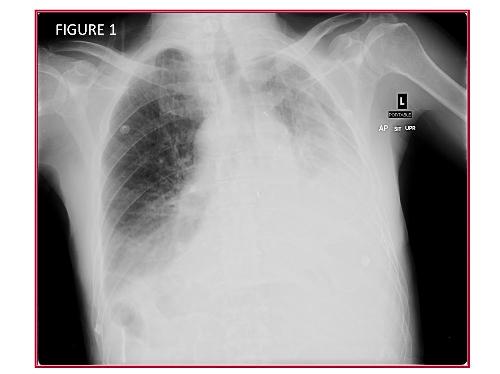
Chest radiography (Figure 1, Panel A) was interpreted as showing a “right upper lobe infiltrate which could represent an acute pneumonia”. No distinct abnormalities were identified on abdominal radiographs (Figure 1, Panel B).
Figure 1. Panel A. Frontal chest radiography. Panel B. Abdominal radiography.
To further evaluate the possibility of a right upper lobe abnormality at chest radiography, thoracic CT was performed and as showing patchy ground-glass opacities throughout the lungs bilaterally (Figure 2).
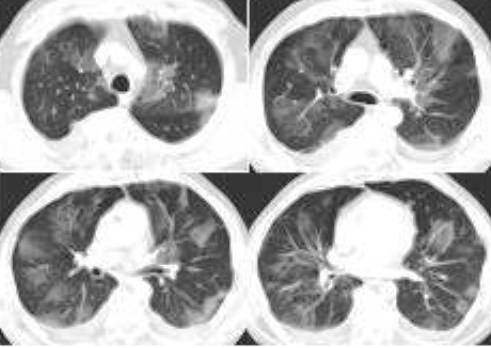
Figure 2. Representative images from thoracic CT.
Question 1. What’s the most likely diagnosis?
- Hypersensitivity pneumonitis
- Acute inhalational injury secondary to “huffing”.
- Drug-induced lung disease
- Valley Fever
- Ground-glass opacities associated with pancreatitis
Question 2. What would you do next?
- Hypersensitivity panel
- Bronchoscopy with bronchoalveolar lavage
- Begin Diflucan
- Broaden his antibiotic coverage
- Repeat the thoracic CT scan in 3-4 days.
The thoracic CT was repeated four days later and the ground-glass opacities seen previously had largely resolved (Figure 3).
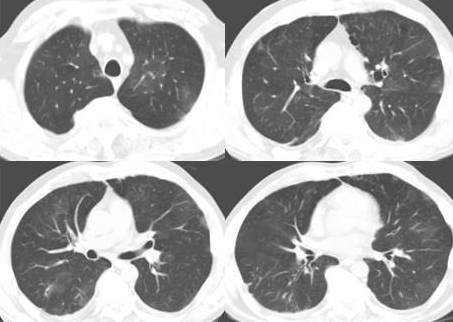
Figure 3. Representative images from thoracic CT performed four days following the initial study Figure 2).
These ground-glass opacities likely represent subclinical non-cardiogenic pulmonary edema in the setting of acute pancreatitis. Ground-glass opacities are foci of increased lung attenuation that do not obscure underlying vessels or bronchial margins (1). Ground-glass opacities often represent parenchymal abnormalities below the spatial resolution of high-resolution CT of the lung. Although the differential diagnosis of ground-glass opacities at high-resolution CT is large, these etiologies may be broadly divided into acute or chronic causes. Table 1 lists some of the more common causes of ground-glass opacities at high-resolution CT.
Table 1: Common Etiologies for Ground-Glass Opacity at Thoracic CT
|
Acute |
Chronic |
|
Pulmonary edema (cardiogenic or non-cardiogenic) |
Interstitial diseases (hypersensitivity pneumonitis, desquamative interstitial pneumonia, respiratory bronchiolitis-interstitial lung disease, nonspecific interstitial pneumonia, sarcoidosis, others) |
|
Infectious pneumonitis (PJP, CMV, HSV, RSV, others) |
Bronchoalveolar carcinoma |
|
Noninfectious pneumonitis (hypersensitivity pneumonitis, acute inhalational exposures, drug-induced lung diseases) |
Other causes (drug toxicity, pulmonary alveolar proteinosis, organizing pneumonia, chroic eosinophilic pneumonia, others) |
Our patient had no apparent cause, other than subclinical non-cardiogenic pulmonary edema secondary to pancreatitis. Pulmonary edema is a well known complication of pancreatitis and can be severe (2). It seems likely that, as more sensitive methods for the detection of pulmonary abnormalities, such as thoracic CT, are increasingly applied to patients with pancreatitis, that subclinical pulmonary injury may be increasingly detected.
Venu Gopal, M.D.
Chief, Infectious Disease, Phoenix VA Medical Center
Richard A. Robbins, M.D.
Chief, Pulmonary and Critical Care, Phoenix VA Medical Center
References
- Miller WT Jr, Shah RM. Isolated diffuse ground-glass opacity in thoracic CT: causes and clinical presentations. AJR Am J Roentgenol 2005;184:613-22.
- Raghu MG, Wig JD, Kochhar R, Gupta D, Gupta R, Yadav TD, Agarwal R, Kudari AK, Doley RP, Javed A. Lung complications in acute pancreatitis. JOP. 2007;8:177-85.