Medical Image of the Month: Cavitating Pseudomonas aeruginosa Pneumonia
 Tuesday, November 2, 2021 at 8:00AM
Tuesday, November 2, 2021 at 8:00AM 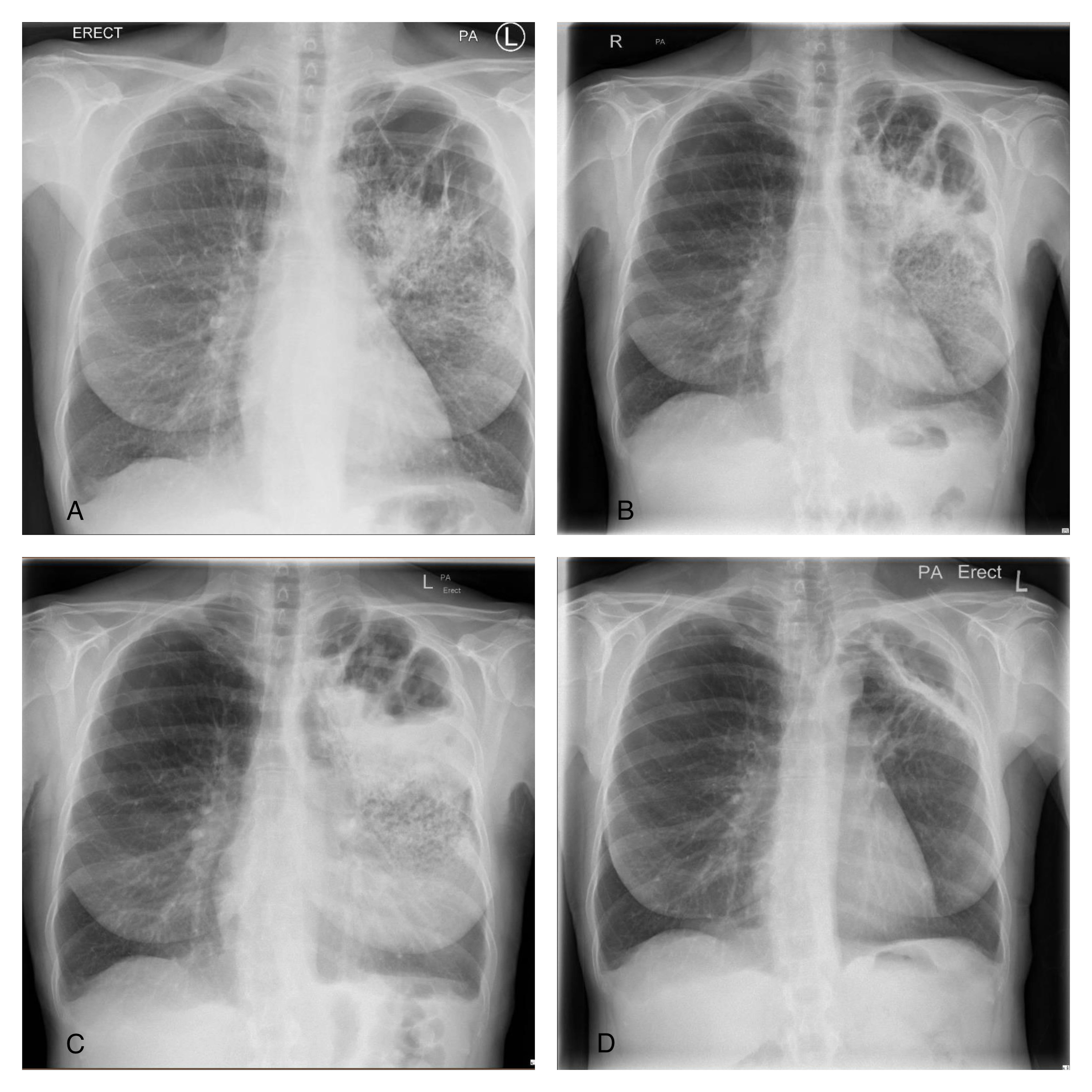
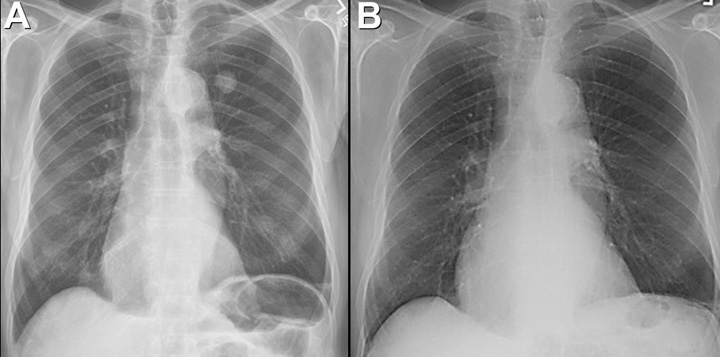
Figure 1. A: Admission CXR demonstrates upper lobe bullae and left peri-hilar consolidation on background of emphysema. B: Day 4 CXR reveals more confluent consolidation and opacification of the bullous change. C: Day 8 CXR demonstrates air fluid level with increasing density of consolidation. D: Repeat CXR 6 weeks after discharge shows near complete resolution of findings with small residual cavity.
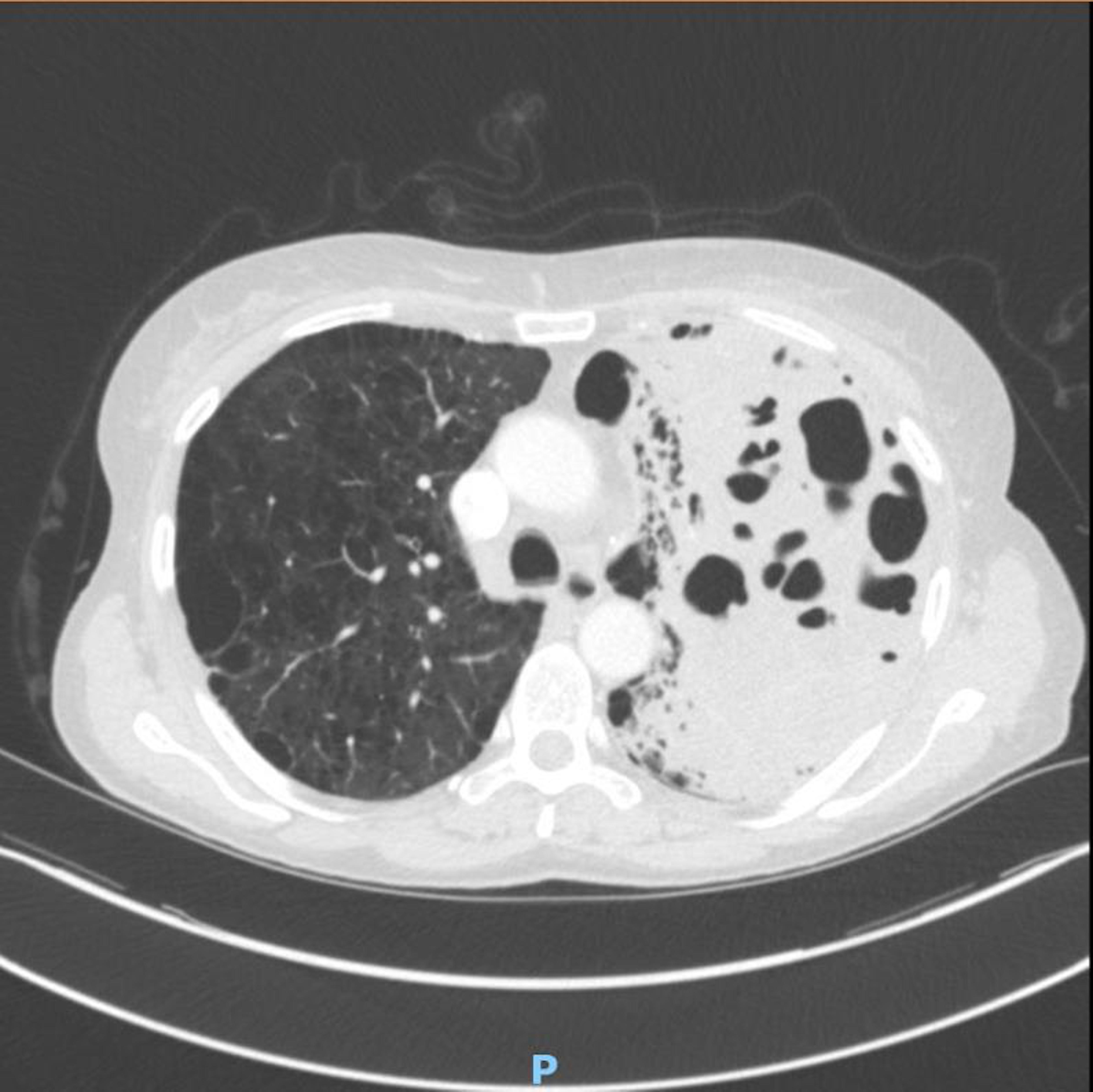
Figure 2. CT Chest with contrast confirmed extensive consolidation with cavitation and suggested possibility of atypical infection
Case Presentation
A 56-year-old woman presented with cough and shortness of breath to hospital. She had a temperature of 39.2°C and had recently completed course of steroids and antibiotics for exacerbation of chronic obstructive pulmonary disease (COPD). She was an active smoker of 15 cigarettes/day for about 40 years. No other past medical history was noted. On examination she had left-sided crepitations and oxygen saturations of 90% on room air.
Chest x-ray (CXR) (Fig 1:A) showed features of background emphysema with upper lobe peripheral bullae, larger on the left. Dense left peri-hilar consolidation was also described. SARS-CoV-2 swab was negative. White blood cells (WBC) were raised at 16.9x109/L and C-reactive protein (CRP) at 331 mg/L. The rest of the blood tests were unremarkable. CURB-65 score was zero but treatment was commenced with intravenous (IV) amoxicillin & oral clarithromycin in view of level of CRP and CXR findings. On Day 4 of admission CRP spiked to 541 mg/L. Repeat CXR (Fig 1:B) showed more confluent left upper zone consolidation and increased opacification of bullous change in the left apex. Microbiologist advised switch of IV Amoxicillin to IV Co-amoxiclav. Respiratory colleagues suggested to check sputum for acid-fast bacilli (AFB). Pneumococcal & legionella urinary antigens came back negative. HIV was also excluded. Growth of Pseudomonas aeruginosa was detected on a blood-tinged sputum sample which was confirmed on 3 more subsequent samples. AFB stain was persistently negative. Blood cultures did not yield any growth.
Antibiotic therapy was escalated to IV piperacillin/tazobactam (Tazocin; Pfizer; UK) QDS (Pseudomonas dose) in light of the new finding. Inflammatory markers slowly started to shift but intermittent temperature spikes continued so repeat CXR (Fig 1:C) and subsequent computed tomography (CT) of chest with contrast (Fig 2) were obtained to assess the complex pneumonia with its striking appearances. CT confirmed extensive consolidation with cavitation and air-fluid levels in the left apical region. Patient required 2L/min supplemental oxygen at the time. By completion of 7-day course of IV piperacillin/tazobactam CRP dropped to 63 mg/L and WBC to 8.6x109/L. Patient was successfully weaned off oxygen and discharged home. Repeat CXR in 6 weeks (Fig 1:D) showed marked improvement with residual small cavity.
Discussion
P. Aeruginosa - a gram negative rod is a rare cause of both CAP (community acquired pneumonia) and cavitating pneumonia. It is more commonly associated with hospital acquired pneumonia (HAP) and usually affects immunocompromised hosts (1). Cavitating pneumonia arises as a result of necrosis of lung parenchyma due to toxins derived from bacterial pathogens. Maharaj et al. (2) reviewed 9 cases of P. Aeruginosa CAP reported on PubMed from 2001 to 2016 and 5 out of 9 patients were found to be smokers. Emphysema was reported in 2 and asthma only in 1 case. The pneumonia exclusively affected upper lobes in 8 out of 9 cases. The infection was fatal in 3 cases (mean age 54) through development of septic shock. Early identification and timely treatment of P. Aeruginosa infection is crucial due to its high rate of multi-drug resistance (3). In absence of positive sputum cultures clinical suspicion based on imaging could drastically change patient’s course of illness. Presentation of upper-lobe pneumonia not responding to standard antibiotic regimens should alert clinicians to the differential of P. Aeruginosa infection. Plain radiograph usually gives sufficient information in CAP but a CT scan may be warranted on an individual basis to assess more complex pneumonia.
Giorgi Kiladze MBcHB, MRCP(UK)
Royal Liverpool and Broadgreen University Hospitals NHS Trust
Prescot Street, Liverpool, Merseyside, UK L7 8XP
References
- Rello J, Borgatta B, Lisboa T. Risk factors for Pseudomonas aeruginosa pneumonia in the early twenty-first century. Intensive Care Med. 2013 Dec;39(12):2204-6. [CrossRef] [PubMed]
- Maharaj S, Isache C, Seegobin K, Chang S, Nelson G. Necrotizing Pseudomonas aeruginosa Community-Acquired Pneumonia: A Case Report and Review of the Literature. Case Rep Infect Dis. 2017;2017:1717492. [CrossRef] [PubMed]
- Wolter DJ, Lister PD. Mechanisms of β-lactam resistance among Pseudomonas aeruginosa. Curr Pharm Des. 2013;19(2):209-22.
Abbreviations
- COPD – Chronic Obstructive Pulmonary Disease
- CXR – Chest X-ray
- WBC – White Blood Cells
- CRP – C Reactive Protein
- CURB 65 – Confusion Urea Respiratory rate Blood pressure Age 65
- IV – Intravenous
- AFB – Acid-Fast Bacilli
- HIV – Human Immunodeficiency Virus
- QDS – Quarter Die Sumendum (four times daily)
- CT – Computed Tomography
- L/min – Litres/minute
- CAP – Community Acquired Pneumonia
- HAP – Hospital Acquired Pneumonia
Cite as: Kiladze G. Medical Image of the Month: Cavitating Pseudomonas aeruginosa Pneumonia. Soulthwest J Pulm Crit Care. 2021;23(5):126-8. doi: https://doi.org/10.13175/swjpcc034-21 PDF