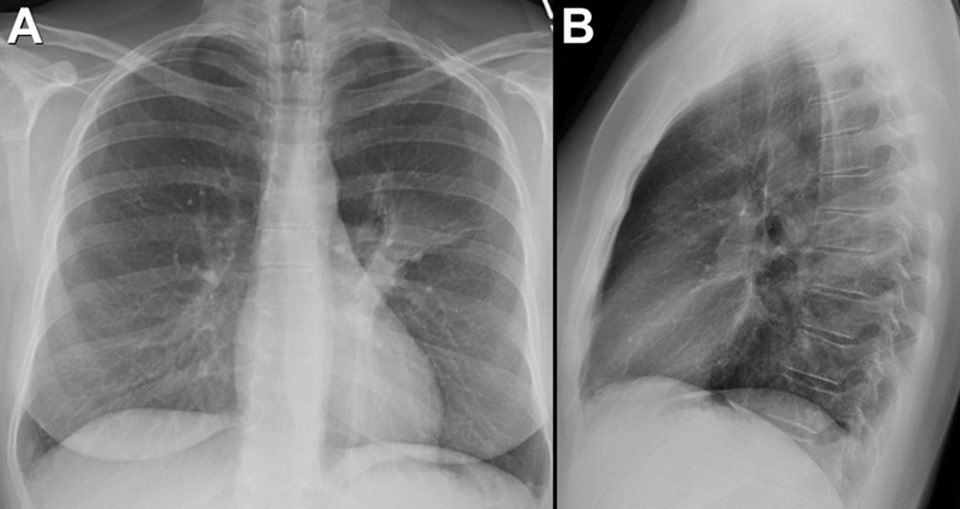
February 2022 Medical Image of the Month: Multifocal Micronodular Pneumocyte Hyperplasia in the Setting of Tuberous Sclerosis
 Wednesday, February 2, 2022 at 8:00AM
Wednesday, February 2, 2022 at 8:00AM 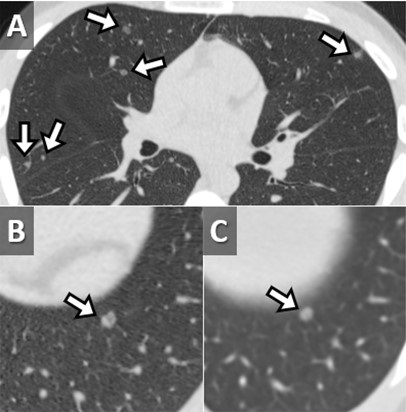
Figure 1. Unenhanced chest CT in the axial (A) plane showing multiple subsolid pulmonary nodules in a random distribution (arrows). Unenhanced chest CT in the axial (A) plane compared to an image from a contrast-enhanced abdominal CT performed 1 year earlier (B) shows relative stability of these nodules (arrows). In a 22 y/o man with known Tuberous Sclerosis Complex, these findings are consistent with Multifocal Micronodular Pneumocyte Hyperplasia. Click here to view Figure 1 in an enlarged window.
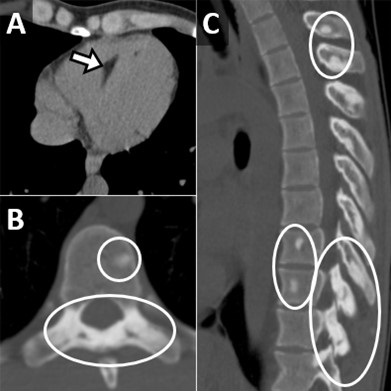
Figure 2. Unenhanced chest CT in the axial (A) plane, soft tissue window display settings, demonstrate foci of myocardial fat (arrow). Unenhanced chest CT in the axial (B) and sagittal (C) planes, bone window display settings, shows multiple small scattered sclerotic osseous foci (circles). These ancillary findings are quite common in the setting of tuberous sclerosis. Click here to view Figure 2 in an enlarged window.
A 22-year-old man with a known diagnosis of Tuberous Sclerosis Complex (TSC) presents for a follow-up unenhanced chest CT to re-evaluate pulmonary nodules seen in the lung bases on a prior abdominal CT. The patient also has a history of multiple renal lesions consistent with lipid-poor angiomyolipomas based on previous abdominal MRI findings. The chest CT demonstrated multiple scattered, randomly distributed sub-centimeter pulmonary nodules of solid or subsolid morphology [Figure 1A]. Those nodules visible in the lung bases on the prior abdominal CT had remined stable over the 12-month interval consistent with multifocal microscopic pneumocyte hyperplasia (MMPH)[Figure 1B,C]. Myocardial fatty foci (MFF) were visualized in the heart on soft tissue window display settings [Figure 2A] as were multiple scattered sclerotic bone lesions on bone window display settings [Figure 2B,C]. No pulmonary cysts were seen to suggest lymphangioleiomyomatosis (LAM) and there were no thoracic lymphangiomas.
MMPH represents a benign hamartomatous proliferation of type II pneumocytes which manifest as small, randomly scattered pulmonary nodules that can be solid or subsolid and are self-limited (1). MMPH is rare in general, but quite common in TSC with a reported incidence as high as 71% (2). MMPH does not demonstrate a sex predilection (unlike LAM in TSC). It is important to remember MMPH in the setting of TSC as it represents a “don’t touch” lesion; recognizing it as such can save unnecessary trouble for the patient (3). The MFF seen on this chest CT also is a relatively common and specific finding in TSC, seen in at least 50% of TSC patients (4,5). Although MMPH and MFF appear to be relatively specific imaging findings in the setting of TSC, as of yet they have not been incorporated into the diagnostic criteria for TSC (6). The small sclerotic bone lesions, especially involving the posterior elements of the spine, are also a well described finding in TSC; however, this finding is much less specific and can be seen in many conditions (7).
Clinton Jokerst MD, Carlos Rojas MD, Prasad Panse MD, Kris Cummings MD, Eric Jensen MD and Michael Gotway MD
Department of Radiology
Mayo Clinic Arizona
Scottsdale, AZ USA
References
- Franz DN, Brody A, Meyer C, Leonard J, Chuck G, Dabora S, Sethuraman G, Colby TV, Kwiatkowski DJ, McCormack FX. Mutational and radiographic analysis of pulmonary disease consistent with lymphangioleiomyomatosis and micronodular pneumocyte hyperplasia in women with tuberous sclerosis. Am J Respir Crit Care Med. 2001 Aug 15;164(4):661-8. [CrossRef] [PubMed]
- Wataya-Kaneda M, Tanaka M, Hamasaki T, Katayama I. Trends in the prevalence of tuberous sclerosis complex manifestations: an epidemiological study of 166 Japanese patients. PLoS One. 2013 May 17;8(5):e63910. [CrossRef] [PubMed]
- Aswani Y, Gavai B. Multifocal micronodular pneumocyte hyperplasia: A "touch-me-not" pulmonary lesion in tuberous sclerosis complex. Lung India. 2018 Sep-Oct;35(5):445-446. [CrossRef] [PubMed]
- Adriaensen ME, Schaefer-Prokop CM, Duyndam DA, Zonnenberg BA, Prokop M. Fatty foci in the myocardium in patients with tuberous sclerosis complex: common finding at CT. Radiology. 2009 Nov;253(2):359-63. [CrossRef] [PubMed]
- Tresoldi S, Munari A, Di Leo G, Pompili G, Magistrelli P, Secchi F, La Briola F, Canevini MP, Cornalba G, Sardanelli F. Myocardial Fatty Foci in Adult Patients with Tuberous Sclerosis Complex: Association with Gene Mutation and Multiorgan Involvement. Radiology. 2015 Nov;277(2):398-405. [CrossRef] [PubMed]
- Northrup H, Krueger DA; International Tuberous Sclerosis Complex Consensus Group. Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 Iinternational Tuberous Sclerosis Complex Consensus Conference. Pediatr Neurol. 2013 Oct;49(4):243-54. [CrossRef] [PubMed]
- Baskin HJ Jr. The pathogenesis and imaging of the tuberous sclerosis complex. Pediatr Radiol. 2008 Sep;38(9):936-52. [CrossRef] [PubMed]