January 2022 Medical Image of the Month: Bronchial Obstruction Due to Pledget in Airway Following Foregut Cyst Resection
 Sunday, January 2, 2022 at 8:00AM
Sunday, January 2, 2022 at 8:00AM 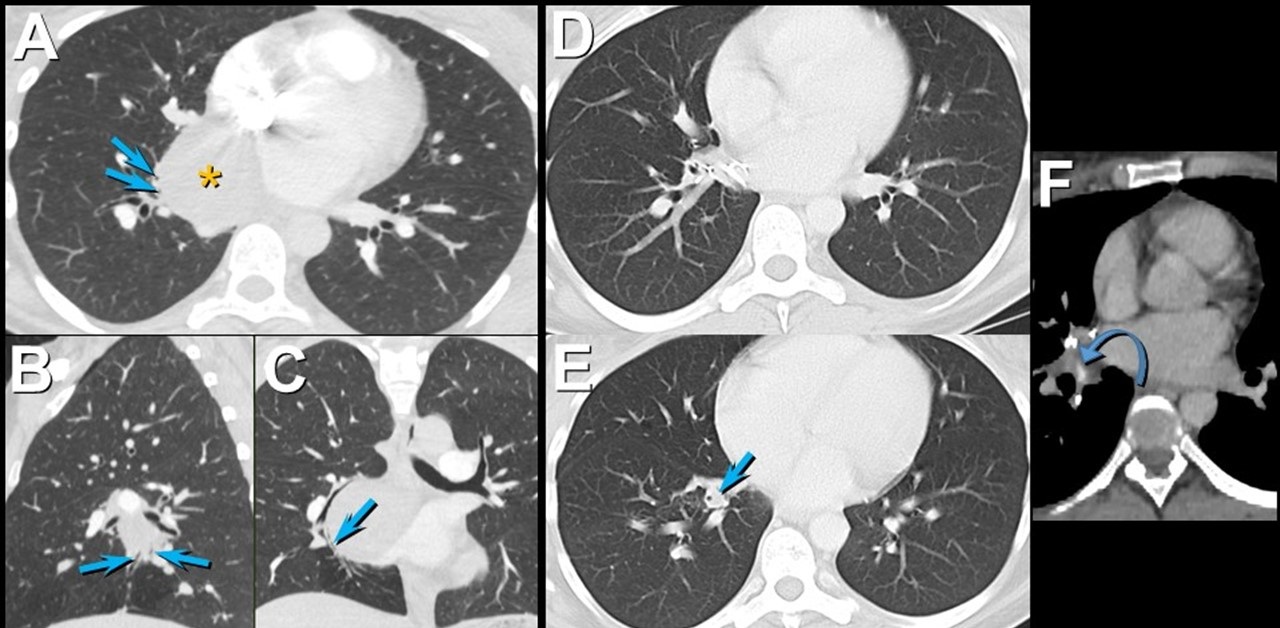
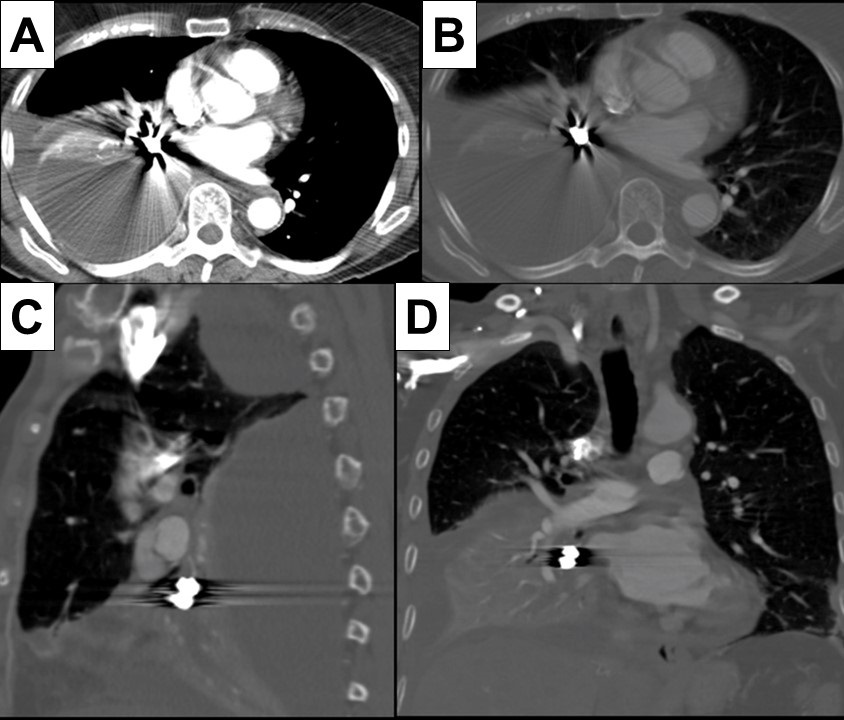
Figure 1. Enhanced chest CT in axial (A), sagittal (B), and coronal (C) planes shows a mediastinal foregut duplication cyst (*) compressing medial basal subsegmental airways (arrows). Axial enhanced chest CT displayed in lung (A and B) and soft tissue (C) windows 7 years after surgical resection of the foregut duplication cyst shows post-resection changes with a focus of hyperattenuation (curved arrow) related to the medial basal segmental bronchus; this bronchus is dilated and fluid-filled more distally (arrow). Click here to view Figure 1 enlarged in a new window.
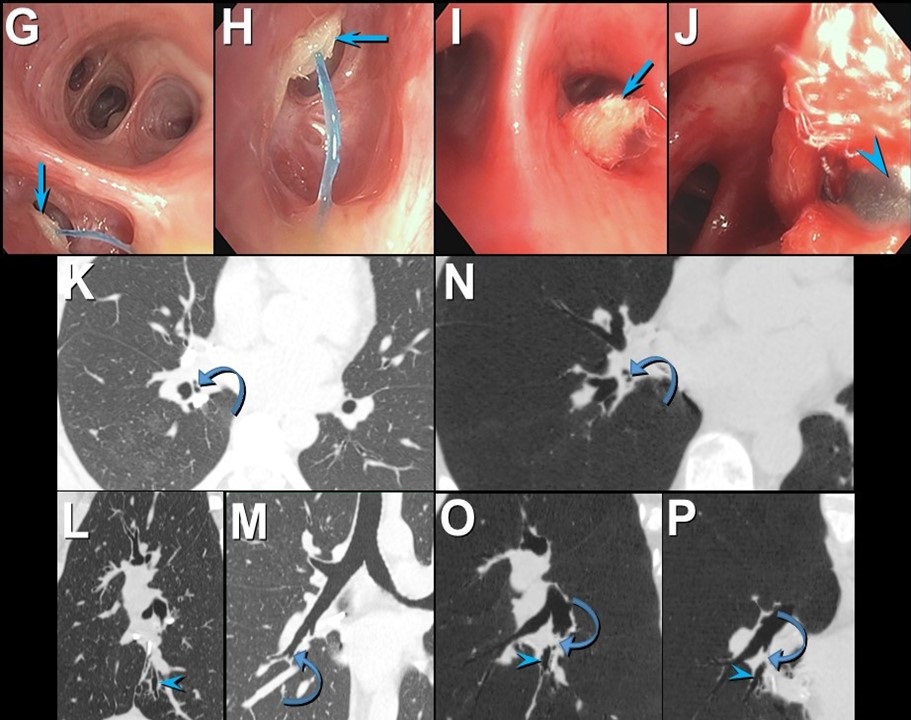
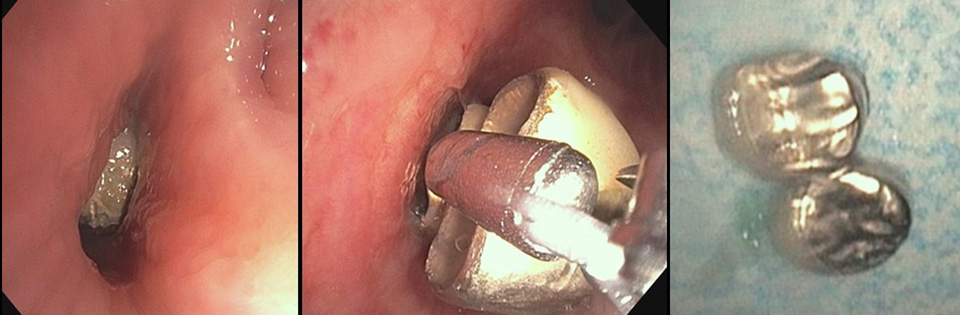
Figure 2. Bronchoscopic images (G-J) show an object obstructing the medial basal segmental right lower lobe bronchus (arrow); a blue suture is attached to the object. The object (arrow) was retrieved using forceps (arrowhead) and was found to reflect a surgical pledget. Follow up unenhanced axial (K), sagittal (L), and coronal (M) chest CT shows mildly stenosed medial basal subsegmental bronchi (curved arrow) with distal bronchiectasis (double arrowheads); these airway abnormalities are shown to advantage using minimum intensity projected images (N-P). Click here to view Figure 2 enlarged in a new window.
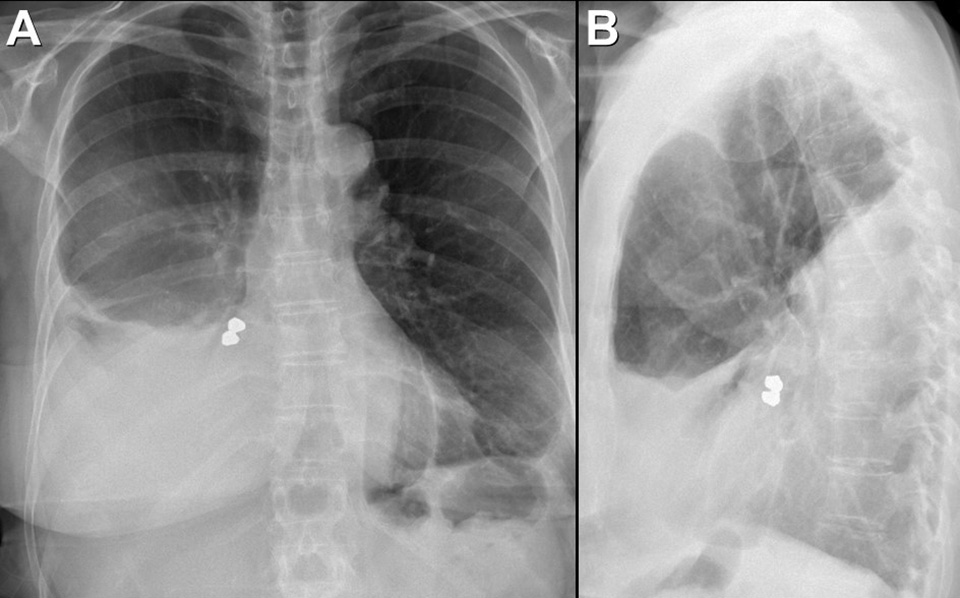
A 37-year-old woman complaining of chest pain and cough underwent resection of a mediastinal foregut duplication cyst complicated by a 10-day hospitalization with a prolonged air leak. Seven years later, she presented with worsening cough and shortness of breath, complaining of similar symptoms intermittently in the 7 years between her surgery and presentation. Chest CT showed a hyperattenuating lesion obstructing the medial basal segmental airways (Figure 1). Bronchoscopy revealed a suture and a pledget obstructing the medial basal segmental right lower lobe bronchus (Figure 2). The pledget and suture were successfully removed. Repeat bronchoscopy several months later showed no residual airway foreign body, although medial basal subsegmental bronchial stenosis prevented advancement of the bronchoscope distally; this finding correlated with the CT impression of airway stenosis or occlusion in this region on the follow up CT.
Bronchogenic cysts result from abnormal lung budding and development of the ventral foregut during the first trimester (1). Many lesions are detected asymptomatically, but larger lesions, as in this patient, may induce symptoms prompting resection. The surgical note for this patient suggested the lesion resided in the right lower lobe, but most bronchogenic cysts arise in the mediastinum near the carina, and this patient’s large lesion extended from the subcarinal space into the azygoesophageal recess. It is possible the surgeon entered the right lower lobe to resect the lesion, resulting in the post-surgical air as well as the surgical pledgets in the medial basal right lower lobe airway that caused the patient’s recurrent chest complaints.
Prasad M. Panse MD1 and Kenneth K. Sakata MD2
Departments of Radiology1 and Pulmonary Medicine2
Mayo Clinic Arizona, Scottsdale, AZ USA
Reference
- Panchanatheeswaran K, Dutta R, Singh KI, Kumar A. Eleven-year experience in thoracoscopic excision of bronchogenic cyst. Asian Cardiovasc Thorac Ann. 2012; 20(5):570-574 perspective. Natl J Maxillofac Surg. 2015; 6(2):144-1451. [CrossRef][PubMed]
Cite as: Panse PM, Sakata KK. January 2022 medical image of the month: bronchial obstruction due to pledget in airway following foregut cyst resection. Southwest J Pulm Crit Care. 2022;24(1):6-7. doi: https://doi.org/10.13175/swjpcc065-21 PDF