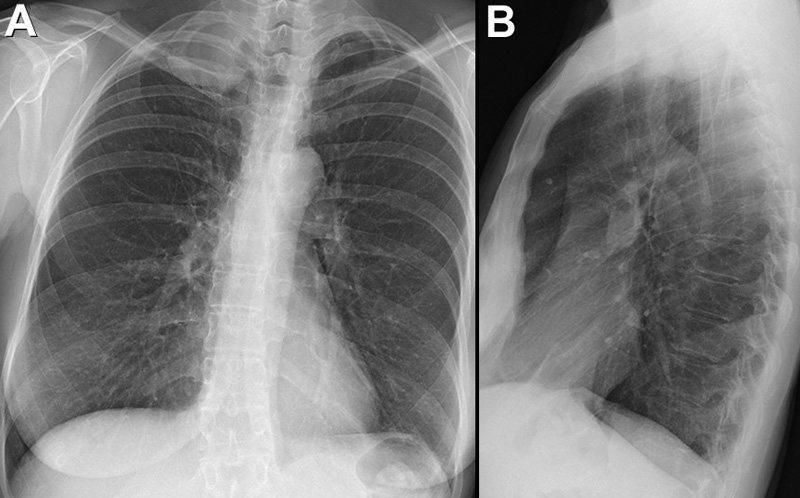
May 2022 Medical Image of the Month: Pectus Excavatum
 Monday, May 2, 2022 at 8:00AM
Monday, May 2, 2022 at 8:00AM 
Figure 1. Thoracic CT in lung windows showing severe pectus excavatum. The distance from the sternum to the vertebral body was 14.7 mm (green line) and the transverse diameter of the chest of 257 mm (red line). This gives a calculated Haller index (shortest AP diameter/transverse diameter) of approximately 17.4.
Case Presentation
A 78-year-old man presented to the emergency department with abdominal discomfort and was ultimately diagnosed with a small bowel obstruction requiring laparoscopic surgery. The patient woke up early in the morning with abdominal pain, which was constant. Nothing alleviated his symptoms. 3 hours later he developed dyspnea and, at that point, went to the hospital. The patient subsequently underwent enhanced commuted tomography of the chest, abdomen, pelvis. Patient was found to have an acute small bowel obstruction and mesenteric swirling and mistiness. Patient was also found to have severe pectus excavatum with the inferior body of the sternum measuring 1.3 cm from the anterior border of T11 vertebral body. General surgery was consulted. Patient ultimately underwent laparoscopic surgery with removal of adhesions and a small bowel serosal tear was repaired. The patient recovered well.
Discussion
Pectus excavatum is a deformity of the chest wall that is characterized by sternal depression. It accounts for 90% of anterior chest wall disorders and treatment and clinical significance depends on severity of chest wall defect, cardiopulmonary morbidity, and psychosocial impact. In severe cases there can be cardiopulmonary impairment. These impairments can worsen as the patient ages. Complications that are associated with pectus excavatum are lung compression caused by the deformity, decreased exercise tolerance, arrythmias such as atrial fibrillation, and mitral valve prolapse. In 20-60% of cases, mitral valve prolapse has also been reported. PFTs that are done on these individuals are significant for a restrictive pattern and patients can have severe exercise intolerance due to this. Indications for operative management include cardiopulmonary impairment and desire to correct defect of the chest due to its appearance. Prior to surgical intervention, the Haller index is used to quantify severity of the deformity and is a ratio of thoracic height and width measured from axial CT image. The Haller index is calculated by dividing the transverse diameter of the chest by the anterior-posterior distance on CT of the chest on the axial slice that demonstrates the smallest distance between the anterior surface of the vertebral body and the posterior surface of the sternum. A significant Haller index is >3.35. For the surgical correction, the preferred operation is the Nuss procedure. It is a minimally invasive procedure and involves placing three bars behind the sternum to hold it in a normal position. In most cases the bars are removed after 3 years. In one study it was noted after Nuss procedure there was a 44% improvement in cardiac stroke volume as well as 40.6% improvement in cardiac output. Furthermore, there was improvement in exercise tolerance following the procedure.
Overall, this is an important topic because pectus excavatum has been seen as a physical deformity, but can have significant impact on cardiac function, pulmonary function, and even psychosocial factors. For example, the presence of pectus excavatum has multiple considerations in the clinical course of the patient. The diminished lung volume places this patient at increased risk of complications with general anesthesia. In this particular patient, the heart rested completely in the right side of the chest. Should a cardiac arrest have occurred, cardiopulmonary resuscitation would have been complicated. Proper resuscitation of this patient would have included right-sided rib compressions rather than sternal placement.
Cameron Barber DO, Jessica Nash DO, Dylan Carroll MD, Karen Randall DO, and Kourtney Aylor-Lee DO
Parkview Medical Center
Pueblo, CO USA
References
- Andre Hebra, MD. “Pectus Excavatum Treatment & Management: Medical Care, Surgical Care, Consultations.” Pectus Excavatum Treatment & Management: Medical Care, Surgical Care, Consultations, Medscape, 8 Nov. 2019, Available at: https://emedicine.medscape.com/article/1004953-treatment#d6 (accessed 3/30/22).
- Das BB, Recto MR, Yeh T. Improvement of cardiopulmonary function after minimally invasive surgical repair of pectus excavatum (Nuss procedure) in children. Ann Pediatr Cardiol. 2019 May-Aug;12(2):77-82. [CrossRef] [PubMed]
- Shaalan AM, Kasb I, Elwakeel EE, Elkamali YA. Outcome of surgical repair of Pectus Excavatum in adults. J Cardiothorac Surg. 2017 Aug 29;12(1):72. [CrossRef] [PubMed]