March 2023 Medical Image of the Month: Spontaneous Pneumomediastinum as a Complication of Marijuana Smoking Due to Müller's Maneuvers
 Thursday, March 2, 2023 at 8:00AM
Thursday, March 2, 2023 at 8:00AM 
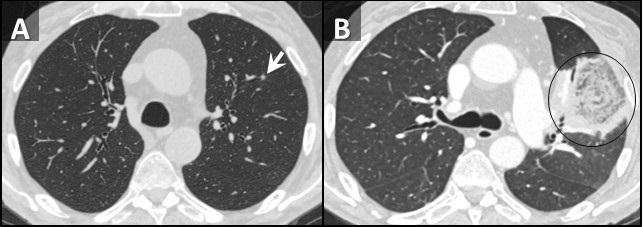
Figure 1. PA chest radiograph obtained at the time of admission (A) demonstrating gas densities (arrows) along left heart border, left paratracheal stripe, upper mediastinum and neck extending into the right supraclavicular fossa in keeping with pneumomediastinum. Follow-up PA chest radiograph performed just before discharge (B) demonstrates resolution of pneumomediastinum.
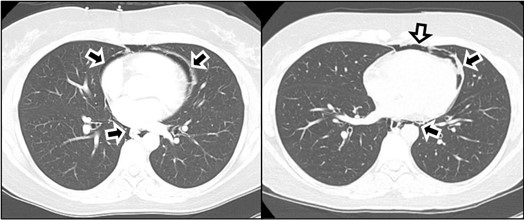
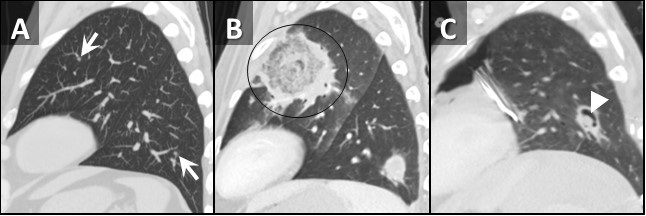
Figure 2. Two axial images through the anterior mediastinum obtained from a contrast-enhanced chest CT demonstrating gas densities (arrows) in the mediastinum anterior to the heart and around the esophagus in-keeping with pneumomediastinum.
A 35-year-old woman with a medical history notable for celiac disease, ulcerative colitis, and bipolar disorder presents to the Emergency Department for evaluation of a strange sensation in the chest and neck associated with nausea and vomiting for one day. The patient also reports persistent nausea and markedly decreased oral intake for the last four days. She reported no concomitant symptoms such as shortness of breath, wheezing, fever, or chills. She denies diarrhea or constipation. Socially, she admits to smoking marijuana daily, and alcohol occasionally.
Vital sign shows blood pressure 147/97 mmHg, pulse 92 BPM, temperature 37.3°C, SpO2 96% breathing ambient air. She appears nontoxic and well-nourished, and the lungs are clear to auscultation bilaterally without any wheezes, rales, or rhonchi. The heart examination reveals a regular rate and rhythm, with normal S1 and S2 heart sounds and no murmurs, rubs, or gallops. The abdomen is soft, non-tender, and not distended. Her extremities do not exhibit any clubbing, cyanosis, or edema. CBC and CMP were unremarkable, and the drug screen test was positive for THC. An ECG is obtained (not shown here), which reveals a normal sinus rhythm with a heart rate of 55 beats/min and no ST-segment or T-wave abnormalities. Chest x-ray and CTA chest, CT abdominal with oral contrast were obtained (Figures 1 and 2). Upon further questioning of the patient’s social history, it was discovered that she smokes marijuana daily using water pipes, and while utilizing a water pipe she attempted a full inspiration against a closed mouth and nose, a technique known as the Müller’s maneuver.
Spontaneous pneumomediastinum (SPM) is a rare condition in which air escapes from the lungs and collects in the mediastinum, the space between the lungs. SPM is almost always a benign, self-limited condition. While SPM can be caused by a variety of factors, including coughing, vomiting, and physical trauma, this case report presents a rare instance of SPM caused by marijuana smoking. Spontaneous pneumomediastinum (SPM) was reported in 1939 by Johns Hopkins clinician Louis Hamman for whom the Hamman sign is named. It is defined as free air or gas contained within the mediastinum, which almost originates from the alveolar space or the conducting airways. Many authors distinguish spontaneous pneumomediastinum as a form of pneumomediastinum that is not associated with blunt force or penetrating chest trauma, endobronchial or esophageal procedures, neonatal lung disease, mechanical ventilation, chest surgery, or other invasive procedures.
The mechanism by which marijuana smoking leads to pneumomediastinum is not well understood, but it is thought to involve increased intra-alveolar pressure and alveolar rupture. This can result in the escape of air into the mediastinum, leading to the development of pneumomediastinum. SPM has been associated with the inhalation of drugs such as cocaine, amphetamines, and marijuana (1-4). Attempted inspiration through a closed glottis or Muller’s maneuver results in a drop in intrathoracic pressure, which increases alveolar air volume, causing alveolar distension and rupture which can cause shear damage and air leakage along a bronchovascular bundle into the mediastinum.
The patient, in this case, was a 35-year-old woman with a history of marijuana smoking who presented with symptoms of chest pain, shortness of breath, and dysphagia. Physical examination revealed subcutaneous emphysema and a chest x-ray confirmed the presence of SPM. This case highlights the potential respiratory complications associated with marijuana smoking, which can lead to SPM and other adverse outcomes. While marijuana use is becoming increasingly common and accepted, it is important for healthcare providers to be aware of the potential risks and to educate their patients about the potential consequences of marijuana use. Further research is needed to understand the full extent of the respiratory effects of marijuana smoking and to develop appropriate interventions and treatments.
Mohammad Abdelaziz Mahmoud DO
Doctors Medical Center of Modesto and Emanuel Medical Center
Modesto and Turlock, CA USA
References
- Weiss ZF, Gore S, Foderaro A. Pneumomediastinum in marijuana users: a retrospective review of 14 cases. BMJ Open Respir Res. 2019 Feb 12;6(1):e000391. [CrossRef] [PubMed]
- Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous pneumomediastinum: diagnostic and therapeutic interventions. J Cardiothorac Surg. 2008 Nov 3;3:59. [CrossRef] [PubMed]
- Puri C, Rhee K, Harish VK, Slack D. Marijuana induced spontaneous pneumomediastinum. J Community Hosp Intern Med Perspect. 2021 Jun 21;11(4):516-517. [CrossRef] [PubMed]
- Motes A, Laoveeravat P, Thongtan T, Nugent K, Islam S, Islam E. Marijuana use-induced spontaneous pneumomediastinum. Proc (Bayl Univ Med Cent). 2020 Dec 7;34(2):274-275. [CrossRef] [PubMed]
Cite as: Mahmoud MA. March 2023 Medical Image of the Month: Spontaneous Pneumomediastinum as a Complication of Marijuana Smoking Due to Müller's Maneuvers. Southwest J Pulm Crit Care Sleep. 2023;26(3):31-33. doi: https://doi.org/10.13175/swjpccs058-22 PDF