November 2022 Medical Image of the Month: COVID-19 Infection Presenting as Spontaneous Subcapsular Hematoma of the Kidney
 Wednesday, November 2, 2022 at 8:00AM
Wednesday, November 2, 2022 at 8:00AM 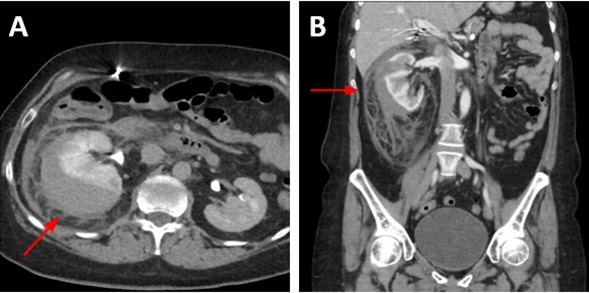
Figure 1. Enhanced abdominal CT images in the axial (A) and coronal (B) reconstruction planes show uniform high attenuation material surrounding the right kidney but conforming to renal shape consistent with subcapsular hematoma (arrows). Note the reactive perinephric stranding in the right retroperitoneal space.
A 57-year-old woman with pertinent medical history of hypertension presented to the emergency department with 3 days of right sided lower abdominal pain radiating to the flank, associated with nausea and nonbloody, nonbilious emesis. She reported recent travel to Florida where she visited amusement parks, but only rode small children’s rides with no experienced physical trauma. She experienced fatigue and chills 5 days prior to presentation and tested positive for SARS-CoV2 virus on admission. She had been vaccinated for COVID-19 x3 (Moderna). No other significant history nor medications were noted, and review of systems was otherwise unremarkable.
Urinalysis demonstrated mild ketonuria (20), proteinuria (100) and moderate hematuria on urinalysis while BUN and creatinine remained stable at baseline throughout. Physical examination confirmed costovertebral angle tenderness to the right side. CT abdomen revealed an American Association for the Surgery of Trauma (AAST) grade 3 right renal subcapsular hematoma with 2.1 cm laceration and striations with a pre-existing right arterial aneurysm. Care was escalated to ICU for closer renal function monitoring; urology and nephrology were consulted for suspected ischemic nephropathy and renal compression with concern for Page (external compression) kidney . After exclusion of traumatic and known causes, interdisciplinary discussion came to the consensus of COVID-19 infection induced SRH.
Subcapsular renal hematoma (SRH) is a challenging medical condition in which hematoma formation may exert pressure on surrounding parenchyma resulting in hypoperfusion or ischemia, with overt concern for rupture with subsequent hemorrhage and hemodynamic instability. While this is a predominantly a medical condition precipitated by neoplasms, abdominal trauma or anticoagulant use, sporadic cases of SRH have been observed since the onset of the COVID-19 pandemic. Here, we present a rare case and imaging of COVID-19 infection induced SRH.
Even three years since the start of the COVID-19 pandemic, clinicians continue to unravel COVID-19’s impact on various body systems. While renal involvement is observed in the form of acute kidney injury in over 30% of hospitalized COVID-19 patients (1), SRH has rarely been documented. Retroperitoneal bleeding from various organs has occurred in COVID-19 patients, but this bleeding is often secondary to prophylactic anticoagulation to combat the suspected inflammation-induced hypercoagulable state (2-4). Seldom does retroperitoneal bleeding occur in the absence of anticoagulant use or other precipitating cause, as is seen in our patient with SRH. Tavoosian et al. (5) illustrate a similar case of an otherwise healthy, COVID-19 positive individual that developed spontaneous subcapsular renal hematoma without history of malignancy, trauma or anticoagulant use. The mechanism by which spontaneous SRH may occur in COVID-19 patients is still unclear. However, our case adds to literature another presentation of spontaneous SRH caused by COVID-19 infection with unique imaging findings and add to the growing differential for causes of SRH and the differential of abdominal pain.
Kally Dey1, Shil Punatar DO2, Tauseef Sarguroh MD2
1 Midwestern University Chicago College of Osteopathic Medicine, Downers Grove, IL USA
2 Franciscan Health Olympia Fields, Olympia Fields, IL USA
References
- Hirsch JS, Ng JH, Ross DW, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98(1):209-218. [CrossRef] [PubMed]
- Patel I, Akoluk A, Douedi S, et al. Life-Threatening Psoas Hematoma due to Retroperitoneal Hemorrhage in a COVID-19 Patient on Enoxaparin Treated With Arterial Embolization: A Case Report. J Clin Med Res. 2020;12(7):458-461. [CrossRef] [PubMed]
- Cattaneo M, Bertinato EM, Birocchi S, et al. Pulmonary Embolism or Pulmonary Thrombosis in COVID-19? Is the Recommendation to Use High-Dose Heparin for Thromboprophylaxis Justified?Thromb Haemost. 2020;120(8):1230-1232. [CrossRef][PubMed]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-1062. Erratum in: Lancet. 2020 Mar 28;395(10229):1038.[CrossRef] [PubMed]
- Tavoosian A, Ahmadi S, Aghamir SMK. Spontaneous perirenal haematoma (SPH) in a COVID-19 patient: A rare case report. Urol Case Rep. 2022 May;42:102006.[CrossRef] [PubMed]
Cite as: Dey K, Punatar S, Sarguroh T. November 2022 Medical Image of the Month: COVID-19 Infection Presenting as Spontaneous Subcapsular Hematoma of the Kidney. Southwest J Pulm Crit Care Sleep. 2022;25(4):67-68. doi: https://doi.org/10.13175/swjpccs041-22 PDF

