More Medical Science and Less Advertising
 Monday, January 28, 2019 at 9:22AM
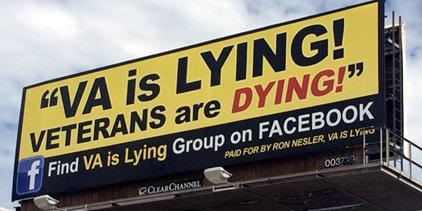
Monday, January 28, 2019 at 9:22AM A recent article appeared in JAMA Open Access reporting that wait times to see a provider in the Department of Veterans Affairs (VA) have improved (1). You might remember that in the not so distant past the VA was embroiled in a controversy for reporting falsely short wait times (2). The widely publicized scandal was centered in Phoenix and led to the firing, resignation or retirement of a number of administrators in VA Central Office, the Southwest Veterans Integrated Service Network (VISN) and the Phoenix VA. What was not as well publicized, but perhaps even more disturbing, was that up to 70% of VA facilities also were reporting deceptively shortened wait times (3). Congress appropriated additional money for the VA to fix the wait times but it is unclear how the money was spent (2).
Now the VA reports that the wait times have shortened and compares favorably to the private sector. The VA’s history has to lead to some skepticism about the data. Is it true? Is it accurate? The short answer is that we do not know because the VA data is largely self-reported. The VA used a different method, the secret shopper approach, for the private sector assessment. In this method a caller requests a routine appointment with a randomly selected care physician in a given health care market. The reported VA data may not be representative of the VA as a whole. Only some metropolitan areas were selected and did not include non-metropolitan facilities and no facilities from the Southwest VISN where there was a known problem. Furthermore, the data is only for new patients requesting a primary care, dermatology, cardiology, or orthopedic appointment. Data for wait times to see other specialties is not reported.
An accompanying editorial by two VA investigators does a good job in explaining the nuances of the study (4). Editorials in response to a specific article are often authored by the reviewers. If these editorial authors were also the article’s reviewers, they can hardly be blamed for saying nice things about the manuscript since “biting the hand that feeds you” is usually a dangerous practice. However, why JAMA published the article in the first place is puzzling. Certainly, lack of timely access to healthcare is very important and lack of access has been associated with higher costs and worse outcomes (4,5). However, this article reports nothing about how the VA achieved this improvement in access. Was it by hiring additional physicians to see the patients or by hiring additional scheduling clerks or additional practice extenders such as physician assistants or nurse practitioners?
The VA data could be easily manipulated. If access by a limited number of new patients is all that is being reported, there may be a tendency to underfund other areas. What about other specialty areas such as oncology, nephrology, pulmonary, neurology, general surgery, ENT, audiology, and ophthalmology to name just a few? What about established patients? What about financial incentives? Were the administrators given bonuses for improving access in these highly selected areas but none or less in others? This is the system the VA used during the wait times scandal and likely contributed to the falsification of data (6).
As it now stands the manuscript represents more advertising than medical science. Medical journals owe their readers better. Hopefully, we at the Southwest Journal are doing a better job of publishing articles that allows the practitioners to better care for their patients and not administrators make their bonus.
Richard A. Robbins, MD
Editor, SWJPCC
References
- Penn M, Bhatnagar S, Kuy S, Lieberman S, Elnahal S, Clancy C, Shulkin D. Comparison of Wait Times for New Patients Between the Private Sector and United States Department of Veterans Affairs Medical Centers. JAMA Netw Open. 2019 Jan 4;2(1):e187096. [CrossRef] [PubMed]
- Wagner D. Seven VA hospitals, one enduring mystery: What's really happening? The Arizona Republic. October 23, 2016. Available at: https://www.azcentral.com/story/news/local/arizona-investigations/2016/10/23/va-hospitals-veterans-health-care-quest-for-answers/90337096/ (accessed 1/25/19).
- 60 Minutes. Robert McDonald: cleaning up the VA. Aired November 9, 2014. Available at: http://www.cbsnews.com/news/robert-mcdonald-cleaning-up-the-veterans-affairs-hospitals/ (accessed 1/25/19).
- Kaboli PJ, Fihn SD. Waiting for Care in Veterans Affairs Health Care Facilities and Elsewhere. JAMA Netw Open. 2019 Jan 4;2(1):e187079. [CrossRef] [PubMed]
- Roemer MI, Hopkins CE, Carr L, Gartside F. Copayments for ambulatory care: penny-wise and pound-foolish. Med Care. 1975 Jun;13(6):457-66. [CrossRef] [PubMed]
- Robbins RA. VA scandal widens. Southwest J Pulm Crit Care. 2014;8(5):288-9.
Cite as: Robbins RA. More medical science and less advertising. Southwest J Pulm Crit Care. 2019;18(1):29-30. doi: https://doi.org/10.13175/swjpcc005-19 PDF
Cite as: Robbins RA