Has the VA Become a White Elephant?
 Friday, November 11, 2016 at 11:00AM
Friday, November 11, 2016 at 11:00AM As I write this Dennis Wagner is publishing a series of articles in the Arizona Republic describing his quest to find out if care at VA hospitals has improved over the last 2 years (1). To begin the article Wagner describes the fable of the King of Siam who presented albino pachyderms to his enemies knowing they would be bankrupted because the cost of food and care outweighed all usefulness. A modern expression derives from this parable: the white elephant.
The Department of Veterans Affairs (VA) has prided itself on being a leader in healthcare. It is the largest healthcare system in the US, implemented the first electronic medical record, and more than 70 percent of all US doctors have received training in the VA healthcare system (2). This year the VA is celebrating the 70th anniversary of its partnership with US medical schools. Beginning in 1946, the VA partnered with academic institutions to provide health care and to train physicians, nurses and other healthcare professionals. “We are extremely proud of the long-standing, close relationships built over the past 70 years among VA and academic institutions across the country” said VA Secretary Robert A. McDonald. “These partnerships strengthen VA’s healthcare system, and provide high quality training for the nation’s healthcare workforce. We cannot do what we do without them.” On this Veterans Day these appear to be empty words.
To understand the VA wait list scandal and why it will be difficult to fix, it is important to understand the history of the VA academic affiliations. The VA initially affiliated with medical schools in 1946 because it had trouble attracting enough quality physicians to staff its hospitals. These affiliations led to the formation of "dean's hospitals" (3). These were VA hospitals closely affiliated with medical schools and made the VA hospitals teaching hospitals. The medical school faculty was in charge of patient care and teaching and the dean's committee oversaw it all. Not surprisingly, these dean's committees were largely despised by the non-physician directors of the VA business offices. In the mid-1990's they persuaded Veterans Health Administration undersecretary, Kenneth W. Kizer, to place them in charge of the VA hospitals as hospital directors. The dean's committees were dissolved, freeing the directors from any real local oversight. This set the foundation for the VA to return to 1945 and a culture that makes it difficult to attract sufficient numbers of quality physicians.
The inability to attract physicians is largely responsible for the widely publicized VA wait time crisis. Although the VA blames their inability to recruit on pay below what the private sector pays, this is only part of the story. VA administrators have repeatedly attempted to direct patient care leading to physician job dissatisfaction and poor morale. Rather than quality healthcare, the VA developed a list of largely meaningless metrics that substituted for quality. These so called "performance-measurements" were favored by VA administration in no small part because of the bonuses they generated for the administrators. This created a cycle of increasing numbers of measurements to generate increasing bonuses. Physicians were often pressured to remind patients to wear seat belts, not keep guns in the home, etc. leaving insufficient time to deal with real and immediate healthcare problems. In retrospect, even Kizer himself called the expanding number of performance measurements "bloated and unfocused" (4).
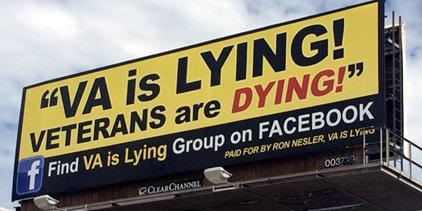
At first VA administrators tried to deny the problem of delayed care due to insufficient staffing. Next VA Central Office tried to make all VA clinics walk-in clinics, essentially shifting the problem to the physicians. When caught in lies about short wait times, VA Secretary McDonald fired a few administrators in Phoenix and then tried to minimize the problem (5). When announcing their progress on the problem, the VA touts the number of people it has hired but usually does not specify the number of physicians or other healthcare providers. Now the VA has decided to let nurses and pharmacists pick up the slack. The VA has proposed removing physician supervision of nurse practitioners and has begun using pharmacists for primary care (6,7).
A number of medical groups have opposed the increased authority for nurses (8). Neither nurses nor pharmacists have the length of training of physicians (9). However, objections by the AMA and other groups are likely to fall on deaf ears. Unless the VA can recruit physician which seems unlikely without reform, what other choice do they have? It is unclear if the VA and courts will hold these less experienced and lower skilled practitioners to the same high standards they have held physicians. However, given that the VA administrators are knowingly replacing physicians with less skilled practitioners, this would seem reasonable.
Wagner's series in the Arizona Republic seems to suggest that the VA's lack of transparency makes it difficult to determine if care at VA hospitals have improved over the last 2 years (9). The conclusion from the series appears to be that the VA has not. This is not surprising given that no real reform has taken place and McDonald appears not to be in control of the VA. For example, two short years ago McDonald was proposing to downsize the VA administration (10). Like so many reforms, this seems to have fallen by the wayside under opposition from VA administration. In fact, Wagner implies that VA administration may actually have grown beyond what was already a bloated bureaucracy (9).
President-elect Trump has been critical of the VA and McDonald. It seems likely he will be gone this January but the VA administrators will remain. Hopefully, McDonald's replacement will do better in reforming the VA. If not, it might be time to view the VA as what it has become, a white elephant whose cost outweighs all usefulness. Consideration should be given to replacing the VA with care in the private sector. Although care will be more expensive, it is better than no or poor care which is what the VA patients are receiving now.
Richard A. Robbins, MD*
Editor, SWJPCC
References
- Wagner D. Seven VA hospitals, one enduring mystery: What's really happening?. Available at: http://www.azcentral.com/story/news/local/arizona-investigations/2016/10/23/va-hospitals-veterans-health-care-quest-for-answers/90337096/ (accessed 10/27/16).
- Department of Veterans Affairs. VA celebrates 70 years of partnering with medical schools. Available at: http://www.va.gov/opa/pressrel/includes/viewPDF.cfm?id=2747 (accessed 10/27/16).
- Department of Veterans Affairs. Still going strong - the history of VA academic affiliations. Available at: http://www.va.gov/OAA/videos/transcript_affiliation_history.asp (accessed 10/27/16).
- Kizer KW, Jha AK. Restoring trust in VA health care. N Engl J Med. 2014 Jul 24;371(4):295-7. [CrossRef] [PubMed]
- Rein L. VA chief compares waits for veteran care to Disneyland: They don’t measure and we shouldn’t either. Washington Post. May 23, 2016. Available at: https://www.washingtonpost.com/news/powerpost/wp/2016/05/23/va-chief-compares-waits-for-veteran-care-to-disneyland-they-dont-measure-and-we-shouldnt-either/ (accessed 10/27/16).
- Department of Veterans Affairs. VA Proposes to grant full practice authority to advanced practice registered nurses. May 29, 2016. Available at: http://www.va.gov/opa/pressrel/pressrelease.cfm?id=2793 (accessed 10/27/16).
- Galewitz P. VA shifts to clinical pharmacists to help ease patients’ long waits. Kaiser Health News. October 25, 2016. Available at: http://khn.org/news/va-treats-patients-impatience-with-clinical-pharmacists/ (accessed 10/27/16).
- Rein L. To cut wait times, VA wants nurses to act like doctors. Doctors say veterans will be harmed. Washington Post. May 27, 2016. Available at: https://www.washingtonpost.com/news/powerpost/wp/2016/05/27/to-cut-wait-times-va-wants-nurses-to-act-like-doctors-doctors-say-veterans-will-be-harmed/ (accessed 10/27/16).
- Robbins RA. Nurse pactitioners' substitution for physicians. Southwest J Pulm Crit Care. 2016;12(2):64-71. [CrossRef]
- Krause J. MyVA re-org likely set to downsize VA workforce, a lot. DisabledVeterans.org. Jan 28, 2015. Available at: http://www.disabledveterans.org/2015/01/29/myva-reorganization-likely-set-downsize-va-workforce-lot/ (accessed 10/27/16).
*The views expressed are those of the author and do not reflect the views of the Arizona, New Mexico, Colorado or California Thoracic Societies or the Mayo Clinic.
Cite as Robbins RA. Has the VA Become a White Elephant? Southwest J Pulm Crit Care. 2016;13(5):235-7. doi: https://doi.org/10.13175/swjpcc108-16 PDF