Healthcare Labor Unions-Has the Time Come?
 Friday, November 3, 2023 at 8:00AM
Friday, November 3, 2023 at 8:00AM Labor unions in America look like they are making a comeback. Employees at Starbucks stores, Amazon warehouses, Trader Joe's, and REI, grad students, Uber and Lyft drivers and employees at the Medieval Times have voted to unionize. Hollywood actors and writers, the United Auto Workers, and Kaiser Permanente employees have been on strike (1). Headline writers began declaring things like, "Employees everywhere are organizing" and that the United States was seeing a "union boom” (2). In September, the White House asserted "Organized labor appears to be having a moment" (2). However, the Bureau of Labor Statistics recently released its union data for 2022 and the data shows that the share of American workers in a union has continued to decline (2). Last year, the union membership rate fell by 0.2 percentage points to 10.1% — the lowest on record.
Despite an increase in union efforts since the pandemic, healthcare workers — particularly doctors — have been slow to join unions. Doctors Council bills itself as the largest physician union in the country with 3500 members according to Joe Crane, national organizing director. However, Crane estimated that only about 3% of US physicians are currently union members. A minority of advanced practice registered nurses (APRNs) (9%) report union membership, according to Medscape's APRN compensation report last year. In a rare alliance, more than 500 physicians, NPs, and PAs at Allina Health primary care and urgent care clinics in Minneapolis, Minnesota, recently filed a petition with the National Labor Relations Board to hold a union election. If successful, the Allina group will join the Doctors Council SEIU, Local 10MD. The Allina healthcare providers share concerns about their working conditions, such as understaffing and inadequate resources, limited decision-making authority, and health systems valuing productivity and profit over patient care.
The economist, Suresh Naidu, and his colleagues have found influential evidence showing that unions played a critical role in boosting wages for American workers and reducing income inequality in the early-to-mid 20th century (3). However, "American labor law just puts an enormous barrier in the way of workers joining a union," Naidu says. "So you need to convince 50% plus one of your coworkers to join a union if you want a union.” That alone can entail a difficult and time-intensive campaign process. Our labor laws make it relatively easy for employers to short-circuit organizing efforts (3). Even when some of their tactics are technically illegal, companies are given wide latitude to thwart unionizing with minimal legal sanctions (3). Union organizers are forced to strategize and organize outside their workplace and figure out how to convince coworkers to join the fight without getting penalized or fired.
The obstacles to forming a union have only grown in recent decades. Around 27 states have passed "Right to Work" laws, which make forming a union more difficult in states with those laws and provide a refuge for companies looking to escape unions in states without those laws (2). Globalization has given companies the option to close-up shop and move overseas. Automation has given companies the option to replace workers with machines. Deregulation has increased industry competition and weakened unions' ability to extract concessions from monopolistic companies. Various changes to labor law, by the U.S. Congress, by state legislatures, and by the federal courts, have made it harder for unions to grow and thrive. Corporations now spend millions and millions on highly paid consultants, developing effective tactics to suppress unionizing efforts and pressure their workers into submission. Once workers form a union, it now takes an average of 465 days for the union to sign a contract with their employer.
Doctors, nurses and healthcare workers tend to underestimate their potential to influence healthcare. If doctors formed a union, many of my colleagues, myself included, would be opposed to an all-out strike since this would likely harm patients. However, the present healthcare system depends on the flow of paperwork with business interests relying on doctors and nurses to generate. Refusing to fill out billing sheets, discharge patients, participate in non-patient care hospital activities are just some of the ways doctors and nurses could impact the system without denying care to patients. A recent strike against Kaiser drove a settlement in 3 days with an increase in wages and an agreement to improve staffing levels (1). The threat of another pandemic and the need for healthcare workers to care for these patients despite chronic understaffing, leaves management backed into a corner.
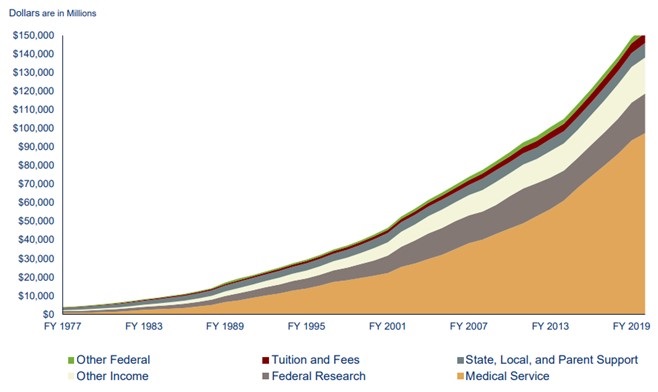
Under these pressures and given the attitude of many doctors and nurses that they are healthcare professionals, not blue-collar workers, it is not surprising that the majority of doctors and nurses are not unionized. However, among my own social group of retired physicians the reluctance to join unions may be waning. One of my most conservative colleagues put it this way, “What choice do we have? Doctors have lost control of medicine and business interests have exploited their control over medicine to take advantage of us and our patients.” Many healthcare workers felt betrayed after the recent COVID-19 pandemic (5). They sacrificed much but received no rewards or even thanks for their sacrifices. Regardless, complaining about the situation is unlikely to change anything. Business interests are unlikely to relinquish control since they are making money, in some cases huge amounts of money. Unions may be one way to reverse the “hyperfinancialization” of medicine and return to a not-for-profit service for patients.
Richard A. Robbins MD
Editor, SWJPCCS
References
- Selena Simmons-Duffin S. After historic strike, Kaiser Permanente workers win 21% raise over 4 years. NPR. October 14, 2023. Available at: https://www.npr.org/sections/health-shots/2023/10/13/1205788228/kaiser-permanente-strike-contract-deal-reached (accessed 10/23/23).
- Rosalsky G. You may have heard of the 'union boom.' The numbers tell a different story. NPR. February 28, 2023. Available at: https://www.npr.org/sections/money/2023/02/28/1159663461/you-may-have-heard-of-the-union-boom-the-numbers-tell-a-different-story#:~:text=Headline%20writers%20began%20declaring%20things,its%20union%20data%20for%202022. (accessed 9/30/23).
- Farber HS, Herbst D, Kuzimenko I, Naidu S. Unions and Inequality over the Twentieth Century: New Evidence from Survey Data. The Quarterly Journal of Economics. 2021; 136 (3):1325–1385. [CrossRef]
- Associated Press. Kaiser Permanente Reaches a Tentative Deal with Health Care Worker Unions After a Recent Strike. October 13, 2023. Available at: https://apnews.com/article/kaiser-permanente-health-care-workers-strike-411aa1f084c19725f29ff87766e99704 (accessed 10/14/23).
- Griffin M, Hamilton P, Harness O, Credland N, McMurray R. ‘Running Towards the Bullets’: Moral Injury in Critical Care Nursing in the COVID-19 Pandemic. J Manag Inq. 2023 Jun 26:10564926231182566. [CrossRef] [PubMed]