Medical School Faculty Have Been Propping Up Academic Medical Centers, But Now Its Squeezing Their Education and Research Bottom Lines
 Thursday, May 5, 2022 at 8:00AM
Thursday, May 5, 2022 at 8:00AM One of my former fellows emailed me an article from Stat+ titled “Hospitals Have Been Financially Propping Up Medical Schools, But Now It’s Squeezing Their Bottom Lines”. The article reports that hospitals have been financially supporting medical schools and are feeling their bottom line squeezed (1). An example cited is the purchase of the University of Arizona Medical Center in Tucson by Banner Health and an agreement by Banner to help both of Arizona’s financially struggling medical schools. Financial statements show that Banner has dedicated roughly $2 billion to the schools and a faculty medical group it bought as part of the 2015 deal. Banner is blaming these expenses for shrinking its operating margin from 5% before the deal to 1% today (1). The businessmen who purchased the academic medical centers initially embraced these mergers but now are facing the financial reality of managing a medical school (1). It seems likely that there will be increasing friction between hospitals and their affiliated medical schools competing for funds. These editorial points out the other side of coin, i.e., that the medical schools are financially shoring up academic medical centers.
Count me as one who is not overly sympathetic to businessmen in charge of academic medical centers. They now collect the pro fees from physicians, paying themselves first. Banner is a good example where the CEO made in excess of $25 million in 2017 compared to the average $155,212 earned by physicians (2). This means the CEO earned more in 2 days than the average physician earned in a year or about $164 for every $1 earned by a physician. As medical education has become more expensive, medical schools now find themselves increasingly reliant on the money they get from their faculty seeing patients and less able to count on other revenue sources, like federal research funding or tuition (Figure 1).
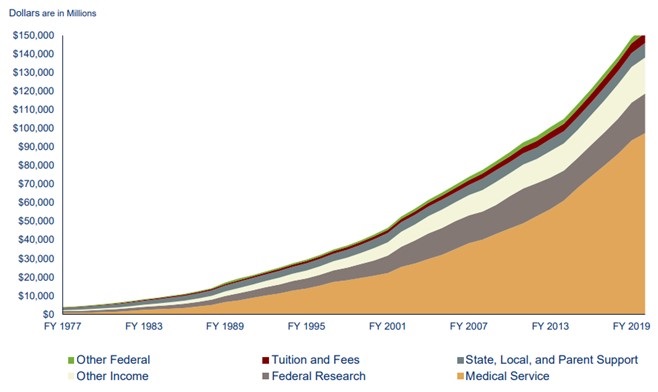
Figure 1. Source of medical school income (1). Click here to view Figure 1 in a new enlarged window.
Furthermore, many physicians, especially pulmonary and critical care physicians, worked above and beyond during the COVID-19 pandemic (3). The pandemic’s resulting disruptions affected academic and educational pursuits such as research productivity, access to mentoring, professional development and networking and personal wellness (3). These disruptions were compounded for faculty at high COVID-19–volume medical centers where clinical responsibilities were necessarily prioritized. Many recognize that it is important to prepare for a postpandemic accelerated burnout syndrome that disproportionately affects early-career physician-scientists at high-volume centers. However, rewards for service have largely been unfulfilled (3).
One quick comment on the validity of hospital ledgers. Physicians are usually shown the finances that businessmen want them to see. The accounting can be prepared to justify further physicians sacrifice of even more time and money. Hospitals tend to see the money generated by physicians, nurses and other healthcare providers as “their” money (1). They see a revenue stream going to a medical school as robbing them of “their” profit and want to know what they get for it (1).
All the above stems from the “hyperfinancialization” of medicine and applying a corporate structure to institutions which should be not-for-profit other than in name only. It is hard to pinpoint an inflection point in medicine, the point in which the direction changed and the mission changed. Maybe it is because in reality the inflection point is not a point but a large blotch, a series of smaller dots in coalesce into a bigger stain brought on by greed. I worry that the core of medicine has been forever damaged; that the doctor patient bond has been replaced with institute/provider - patient service. This model has proven to be more costly, less rewarding and associated with higher burnout. Yet, we continue to move forward with this model. Mergers between community-based physicians and hospitals which are supposed to bridge the gap between evidenced-based care and practice-based care has only served to devalue the intangibles in medicine further, always looking for what can be standardized and more importantly… billable. A corporate structure with a board, CEO, and a variety of vice presidents and other corporate titles has not served the public well. Physicians make less, administrators make more and hospital services have declined or not improved (4). One needs to only look at outcomes such as life expectancy and costs as a percent of GNP (gross National product) to recognize there is a problem (5).
Many, including myself, remain skeptical of the intrusion of business interests into medical education. The oversight of academic medical centers provided by organizations such as the Accreditation Council for Graduate Medical Education (ACGME) that protects the public’s interests remain inadequate. Presently only a written statement must be provided every 5 years that “documents the Sponsoring Institution’s commitment to education by providing the necessary financial support for administrative, educational, and clinical resources, including personnel.” This is to be reviewed, dated, and signed by the designated institutional official (DIO), a representative of the Sponsoring Institution’s senior administration, and a representative of the Governing Body (6). It seems unlikely that review every 5 years by a DIO and other officials employed and dependent on medical center support is likely sufficient.
To provide oversight I recommend that a system be developed to hold medical center administrators accountable for decisions that lead to a decline in efficiency at both in the medical center and their affiliated medical schools (4). If they are in charge of medical care as they seem to think they are, then deficiencies need to be laid at their feet - the same for medical education and research. After all they now credential the healthcare providers and any deficiencies would seem to have resulted from a poor work environment or poor administrative judgment in credentialing. It is time that administrators are held to the same standard. Physicians are required to have continued medical education, board certifications, etc. for credentialling. Present hospital systems where a board elects its own members with the nomination and blessing by the hospital CEO need to end. The chief of staff should be elected by the hospital staff and the majority of members of a hospital board need to be independent of the CEO and knowledgeable about the practice of medicine at that medical center (7). If administrators are not acting in a manner that promotes the doctor patient bond, increases the access to care, promoting cost containment in a transparent manner, and promote physician well-being, then it is time for them to go.
Richard A. Robbins MD
Editor, SWJPCCS
References
- Bannow T. Hospitals have been financially propping up medical schools, but now it’s squeezing their bottom lines. Stat+. April 14, 2022. Available at: https://www.statnews.com/2022/04/14/hospitals-medical-schools-financial-relationship-tension-squeezing-bottom-line/ (requires subscription).
- Robbins RA. CEO compensation-one reason healthcare costs so much. Southwest J Pulm Crit Care. 2019;19(2):76-8. [CrossRef]
- Kliment CR, Barbash IJ, Brenner JS, Chandra D, Courtright K, Gauthier MC, Robinson KM, Scheunemann LP, Shah FA, Christie JD, Morris A. COVID-19 and the Early-Career Physician-Scientist. Fostering Resilience beyond the Pandemic. ATS Sch. 2020 Oct 23;2(1):19-28. [CrossRef] [PubMed]
- Jeurissen PPT, Kruse FM, Busse R, Himmelstein DU, Mossialos E, Woolhandler S. For-Profit Hospitals Have Thrived Because of Generous Public Reimbursement Schemes, Not Greater Efficiency: A Multi-Country Case Study. Int J Health Serv. 2021 Jan;51(1):67-89. [CrossRef] [PubMed]
- Cohen J. Dismal U.S. Life Expectancy Trend Reflects Disconnect Between Dollars Spent On Healthcare And Value Produced. Forbes. Nov 1, 2020. Available at: https://www.forbes.com/sites/joshuacohen/2020/11/01/dismal-us-life-expectancy-trend-reflects-disconnect-between-dollars-spent-on-healthcare-and-value-produced/?sh=3657f353847e (accessed 5/2/22).
- Accreditation Council for Graduate Medical Education. Institutional Requirements. Available at: https://www.acgme.org/globalassets/pfassets/programrequirements/800_institutionalrequirements2022.pdf (accessed 5/2/22).
- Robbins RA. Time for a Change in Hospital Governance. Southwest J Pulm Crit Care Sleep. 2022;24(3):43-5. [CrossRef]
