November 2023 Imaging Case of the Month: A Crazy Association
 Wednesday, November 1, 2023 at 8:00AM
Wednesday, November 1, 2023 at 8:00AM Parker J. Brown MD, Prasad M. Panse MD and Michael B. Gotway MD
Department of Radiology
Mayo Clinic, Arizona
Phoenix, Arizona
HPI: A 55-year-old man presents with a history of cough, poor appetite, low energy, and weight loss over the previous 6-10 months following COVID-19 infection 2 months earlier.
PMH, SH, FH: The patient’s past medical history was positive for CVOID-19 infection 2 months earlier as well as pneumonia, not specified, in the previous year.
The patient’s past medical history was also remarkable for a 7-unit gastrointestinal hemorrhage approximately one year earlier following polypectomy for benign lesions in the transverse colon. During that hospital admission a complete blood count showed 1% blasts which prompted hematology consultation. The consulting oncologist felt the peripheral blasts were the result of a leukemoid reaction secondary to increased bone marrow stimulation owing to the patient’s acute anemia caused by the gastrointestinal hemorrhage. Macrocytosis and reticulocytosis was also noted and attributed to the same. Repeat complete blood count showed no blasts although some myelocytes, metamyelocytes, and polychromasia was noted for which follow up assessment was recommended. Serum B12 and folate levels were normal.
The patient had no prior surgeries.
The patient was not taking any prescription medications.
The patient is a non-smoker. He has no known allergies and drinks alcohol only socially and denied illicit drug use.
There was no significant family history.
Physical Examination: The patient’s physical examination showed his temperature to be 96.7°F with borderline elevated pulse rate of 95/min, a normal respiratory rate, and blood pressure of 118/67 mmHg. Room air oxygen saturation was 98%.
Initial Laboratory: A complete blood count showed a normal white blood cell count at 5.6 x109/L (normal, 3.4 – 9.6 x109/L), with 75% bands (normal, 50-75%). His hemoglobin and hematocrit values were 10.1 gm/dL (normal, 13.2 – 16.6 gm/dL) and 31.6% (normal, 38.3 – 48.6%). The platelet count was normal at 225 x 109/L (normal, 135 – 317 x 109/L). The patient’s serum chemistries and liver function studies were normal aside from mildly decreased total protein at 5.7 gm/dL (normal, 6.3-.9 gm/dL). The patient had an elevated anti-nuclear antibody titer at 1:320. SARS-CoV-2 PCR testing was positive.
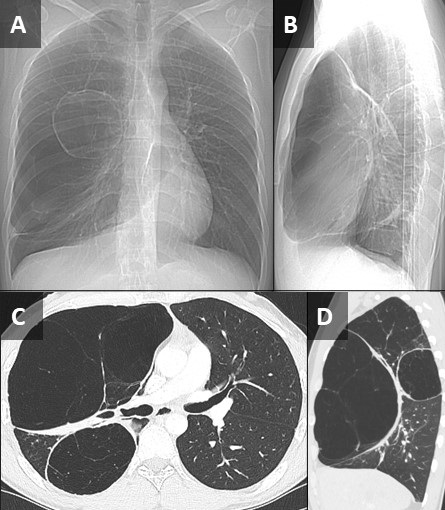
Radiography: Frontal chest radiography (Figure 1) was performed.
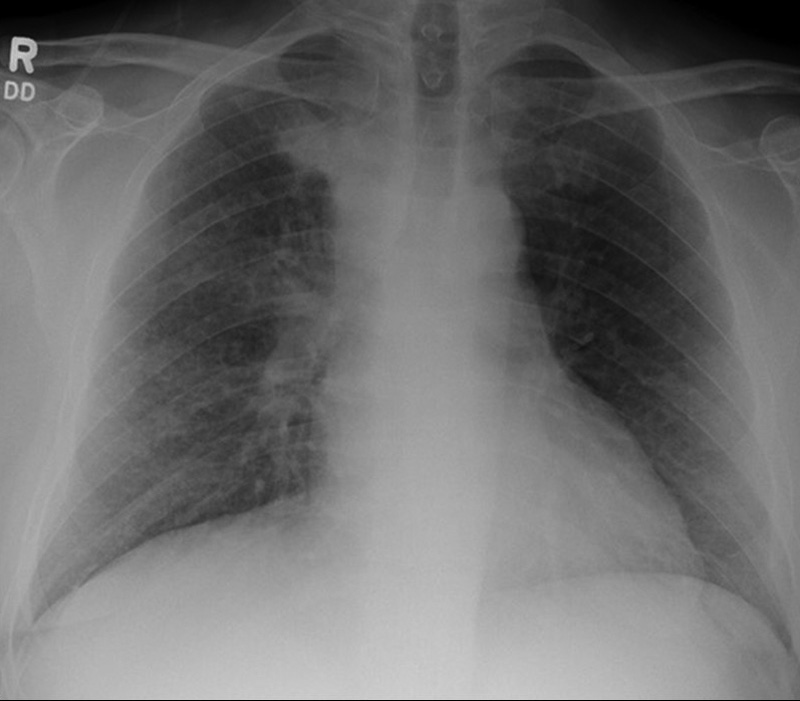 Figure 1. Frontal chest radiography at presentation.
Figure 1. Frontal chest radiography at presentation.
Which of the following statements regarding this chest radiograph is accurate? (Click on the correct answer to be directed to the second of fourteen pages).
- Frontal chest radiography shows normal findings
- Frontal chest radiography shows marked cardiomegaly
- Frontal chest radiography shows mediastinal lymphadenopathy
- Frontal chest radiography shows pleural effusion
- Frontal chest radiography shows multifocal consolidation