Doctor or Money Shortage in California?
 Saturday, July 20, 2019 at 6:20PM
Saturday, July 20, 2019 at 6:20PM An LA Times article titled “California doesn’t have enough doctors. To recruit them, the state is paying off medical school debt” describes a program where the State of California will pay off student debts using Proposition 56 tobacco tax revenue (1). California’s program is aimed at increasing the number of doctors who see Medi-Cal patients which has not kept pace with the rapid expansion of the state’s healthcare program for the poor, which now covers 1 in 3 residents in the state. The trends of decreasing doctors who accept Medi-Cal along with the increasing number of Medi-Cal patients led healthcare, education and business leaders to form the California Future Health Workforce Commission (CFHWC) in 2017 to study the state’s impending healthcare crisis (2). The CFHWC task force ultimately proposed a $3-billion plan over the next 10 years including $120 million for loan forgiveness incentives that’s meant to ensure physicians and dentists take on Medi-Cal patients. Another component of the program would allow nurse practitioners to practice independently from physicians.
The program is telling of both education and reimbursement in California. The CFHWC task force states that California is experiencing a shortage of doctors (3). This is not true. It is true that the graduation of doctors has not kept pace with the expanding California population. The national average of medical school students per 100,000 people is 30.3; California has 18.4 students per 100,000 (1,3). That’s the third-lowest rate among the 45 states that have at least one medical school. California has made relatively few investments in increasing enrollment at medical schools in the state. The only new public medical school to open in California in the last four decades is at UC Riverside and class size has only slightly expanded in the other schools (1,3). At the same time, more than one-third of the state’s doctors and nurse practitioners are reaching retirement age (1).
More than 60% of California’s students who attended medical school in 2017 left the state for their residency, according to the commission’s report. Most doctors settle near their residencies and California must expand the number of residency positions offered according to the CFHWC task force (1,3). They added that the state has historically underfunded those programs (1,3).
Despite these deficiencies, California does not have a shortage of doctors compared to other states (Table 1).
Table 1. Number of physicians per 100,000 population (Phys/105 Pop) by state (2016 data, 4).
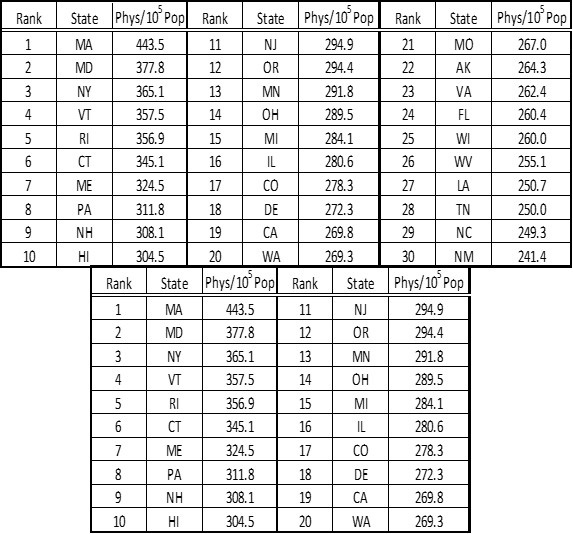
In 2016 California ranked nineteenth of the fifty states in numbers of physicians per 100,000 population (4). In addition, it ranked 22nd in active primary care physicians (4).
What the CFHWC task force really means (and says intermittently) is that the number of doctors willing to accept Medi-Cal payment is low. The reason for this is pretty simple, Medi-Cal reimbursement is abysmally small. For a routine office call (CPT code 99213) Medi-Cal reimburses $24.00 (5). This office code is for about 15 minutes of patient contact and must include: 1. an expanded problem focused history, 2. an expanded problem focused examination, and 3. medical decision making of low complexity. This might be difficult to accomplish in 15 minutes. Documentation and billing would require at least 5 minutes more if the physician is a lightning fast typist. In contrast, Medicare pays $77.72 and Arizona Health Care Cost Containment System (AHCCCS) Administration (Arizona’s Medicaid) pays $51.42. Income generated from a busy practice seeing only Medi-Cal patients at $24.00 per office visit would mean $72/hour, about $500/day (7 hours/day), $2500 per week ($500/day X 5 days a week) or about $120,000/year (48 weeks). Although office overhead (payroll, rent, vendors, information technology, insurance, office equipment, etc.) varies widely, in 2002 the average general internist’s office overhead was about $250,000 (6). Expenses have not likely decreased in the last 16 years meaning that under the very best of circumstances, a physician seeing only Medi-Cal patients would lose $130,000/year serving California’s poor.
Medi-Cal has seemed to attempt to place the financial burden of caring for the poor on physicians and nurse practitioners rather than solving the problem of low reimbursement. Recent residency graduates who agree to have their debt relieved by California in exchange for seeing Medi-Cal patients may find their debt increasing under California’s proposal. Cuts could be made in other areas (hospital costs, drugs, etc.) but ultimately it seems that adequate reimbursement will be necessary to solve the impending “healthcare crisis”.
Richard A. Robbins, MD
Editor, SWJPCC
References
- Gutierrez M. California doesn’t have enough doctors. To recruit them, the state is paying off medical school debt. LA Times. July 16, 2019. Available at: https://www.latimes.com/politics/la-pol-ca-california-doctor-shortage-medical-debt-20190716-story.html (accessed 7/19/19).
- Gutierrez M. $3 billion is needed to address California’s doctor shortage, task force says. LA Times. February 5, 2019. Available at: https://www.latimes.com/politics/la-pol-ca-california-future-health-workforce-commission-doctor-shortage-20190205-story.html (accessed 7/19/19).
- Mijic V. Meeting the demand for health: fact sheet on California’s looming workforce crisis. California Future Health Workforce Commission. February 4, 2019. Available at: https://futurehealthworkforce.org/2019/02/04/ca-looming-workforce-crisis/ (accessed 7/19/19).
- American Association of Medical Colleges. 2017 State Physician Workforce Data Report. Available at: https://store.aamc.org/downloadable/download/sample/sample_id/30/ (accessed 7/19/19).
- Department of Healthcare Services Medi-Cal. Medi-Cal rates as of 07/15/2019 (codes 94799 thru 99600). Available at: https://files.medi-cal.ca.gov/pubsdoco/rates/rates_information.asp?num=22&first=94799&last=99600 (accessed 7/19/19).
- Weiss GG. Expense survey: what it costs to practice today. Med Econ. 2002 Dec 9;79(23):36-8, 41. [PubMed]
Cite as: Robbins RA. Doctor of money shortage in California? Southwest J Pulm Crit Care. 2019;19(1):15-7. doi: https://doi.org/10.13175/swjpcc050-19 PDF
