Improving Quality in Healthcare
 Friday, January 13, 2023 at 8:00AM
Friday, January 13, 2023 at 8:00AM 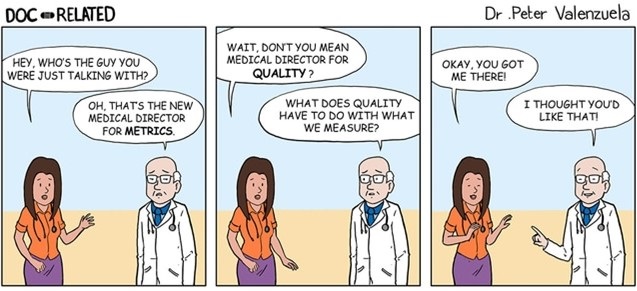
Figure 1. Dr. Katz is a little jaded about quality metrics (1).
Everyone is in favor of quality healthcare and improving it. However, to date, initially highly touted quality measures prove to be meaningless metrics in about 5-10 years. That is, when the measures are scientifically studied, they are found to be of little worth. The cycle is then repeated, i.e., new and highly touted measures are again selected and found to be useless in 5-10 years. The latest in this cycle may be the Centers for Medicare and Medicaid’s (CMS) Merit-based Incentive Payment System (MIPS). The theory underlying MIPS has been that paying for quality rather than quantity will incentivize healthcare providers to improve quality. As part of the deal creating the Affordable Care Act (Obamacare) MIPS was established as a pay for performance system which promised to improve healthcare while reducing costs. However, healthcare costs have continued to rise (2). Data on improvement in quality has been lacking.
Now, Bond et al. (3) have reported a study suggesting that MIPS incentivization of quality improvement in healthcare quality has questionable benefits. Among US primary care physicians in 2019, MIPS scores were inconsistently associated with performance on process and outcome measures. Bond’s study included 3.4 million patients attributed to 80,246 primary care physicians. Physicians were divided into thirds based on their MIPS score. Compared with physicians with high MIPS scores, physicians with the lowest MIPS scores had significantly worse mean performance on 3 of 5 process measures: diabetic eye examinations, diabetic HbA1c screening and mammography screening, but significantly better mean performance on rates of influenza vaccination and tobacco screening. MIPS scores were inconsistently associated with risk-adjusted patient outcomes: compared with physicians with the highest MIPS scores, physicians with the lowest MIPS scores had significantly better mean performance on emergency department visits per 1000 patients but worse performance on all-cause hospitalizations, and did not have significantly different performance on 4 ambulatory care-sensitive admission outcomes. Nineteen percent of physicians with the lowest MIPS scores had composite outcomes performance in the top quintile, while 21% of physicians with the highest MIPS scores had outcomes in the bottom quintile. These findings suggest that the MIPS program may be ineffective at measuring and incentivizing quality improvement among US physicians.
It is unclear why improvement in intermediate surrogate markers is used rather than improvement in outcomes. Bond’s study measured MIPS scores against ER visits and hospitalizations. Patients, providers, insurers, bureaucrats, politicians, taxpayers- in other words, nearly everyone- would agree that reductions in ER visits and hospitalizations is desirable if it can be accomplished without patient harm. Similarly, reduction in unexpected deaths and improvement in patients’ feeling of well being are goals that all can support. However, the goals of healthcare are different depending on which population is asked. Patients might support their well-being, insurance cost, and provider access as being most important, whereas payors might support costs as most important. Providers might support efficiency of care and reimbursement as important. So ultimately what surrogate markers like MIPS do is choose one point of view which often does not affect outcomes (4).
There are many ways to achieve a goal depending on expertise, resources and patient characteristics. Flexibility in care allows the person most likely to understand the efficiencies of their particular system- the providers- to use their local knowledge to benefit the patients. Outside influences emphasizing surrogate markers, cost, or politics have historically failed. Unless one is willing to accept healthcare shown not to benefit patients as acceptable, MIPS should be eliminated. Replacing MIPS with an equally flawed system set of surrogate markers will likely not help.
It seems that outcome measures offer several advantages over process measures. Outcome measures include unexpected mortality, hospital readmissions, safety of care, effectiveness of care, timeliness of care, efficiency of care, and patient well-being (5). These are all thought to be important by patients, insurers, providers and even politicians. In my view, the process leading to these ultimate outcome goals is less important and the process producing the same or similar results will likely vary between providers and hospitals.
CMS should refocus their quality efforts on outcomes rather than processes which have failed as quality indicators. Physicians must decide whether they wish to continue participation in systems such as MIPS and the accompanying increase in paperwork. Unless something changes the trends of increasing paperwork over meaningless metrics will continue.
Richard A. Robbins MD
Editor, SWJPCCS
References
- Lehmann C. Comics for Docs: Medical Cartoons Poke Fun at Today's Practices. Medscape. July 15, 2022. Available at: https://www.medscape.com/slideshow/medical-cartoons-6015473#2 (accessed (1/12/23).
- Kurani N, Ortaliza J, Wager E, Fox L, Amin K. How Has U.S. Spending on Healthcare Changed Over Time? Peterson-KFF Health System Trasecker. February 25, 2022. Available at: https://www.healthsystemtracker.org/chart-collection/u-s-spending-healthcare-changed- time/#Total%20national%20health%20expenditures,%20US%20$%20Billions,%201970-2020 (Accessed 1/4/23).
- Bond AM, Schpero WL, Casalino LP, Zhang M, Khullar D. Association Between Individual Primary Care Physician Merit-based Incentive Payment System Score and Measures of Process and Patient Outcomes. JAMA. 2022 Dec 6;328(21):2136-2146. [CrossRef] [PubMed]
- Robbins RA, Thomas AR, Raschke RA. Guidelines, recommendations and improvement in healthcare. Southwest J Pulm Crit Care. 2011;2:34-37.
- Tinker A. The Top Seven Healthcare Outcome Measures and Three Measurement Essentials. Health Catalyst. June 29, 2022. Available at: https://www.healthcatalyst.com/insights/top-7-healthcare-outcome-measures (accessed 1/5/23).
Cite as: Robbins RA. Improving Quality in Healthcare. Southwest J Pulm Crit Care Sleep. 2023;26(1):8-10. doi: https://doi.org/10.13175/swjpccs002-23 PDF
