What Will Happen with the Generic Drug Companies’ Lawsuit: Lessons from the Tobacco Settlement
 Monday, June 3, 2019 at 8:51AM
Monday, June 3, 2019 at 8:51AM The State Attorney General of Connecticut, William Tong, has sued generic drug companies claiming they conspired to inflate prices and defraud the public of billions of dollars (1). To date, 43 state attorney generals have joined the suit. Tong, who takes doxycycline for rosacea, saw the price increase from $20 for 500 tablets in 2013 to $1,829 a year later. Although several generic companies sell doxycycline, one of the largest is Mylan. Both Mylan and their CEO, Heather Bresch, became infamous for the $10,000 EpiPen and a 4000% price hike in albuterol after testifying before the Senate Judiciary Committee in 2016 (2). The committee took no action and itself came under scrutiny when it was revealed that Mylan had made substantial campaign contributions to nearly all members of the committee (2). Other companies named in this lawsuit include Teva, Sandoz, Pfizer and 16 other drug manufacturers.
Now the states’ attorney generals, like knights on their shining armor, are rushing to protect the public from these “evil generic drug company price gougers.” The present suit is reminiscent of a prior generation of states’ attorney generals who 20 years ago filed and eventually settled a lawsuit against tobacco manufacturers for $206 billion (not a typo that is b as in billion) over 25 years (3). Based on that Tobacco Settlement we can predict what will happen with the generic drug company lawsuit. After legal wrangling for several years, a settlement of at least several billion will be reached. Payments will be placed in the states’ general funds. Like the tobacco companies, the drug companies will negotiate as a condition of the settlement to continue their business largely unregulated.
In 2007, the Government Accountability Office (GAO) reported that 22.9 % of proceeds from the Tobacco Settlement had gone to close state budget shortfalls, often to make up deficits caused by tax cuts (Figure 1) (3).
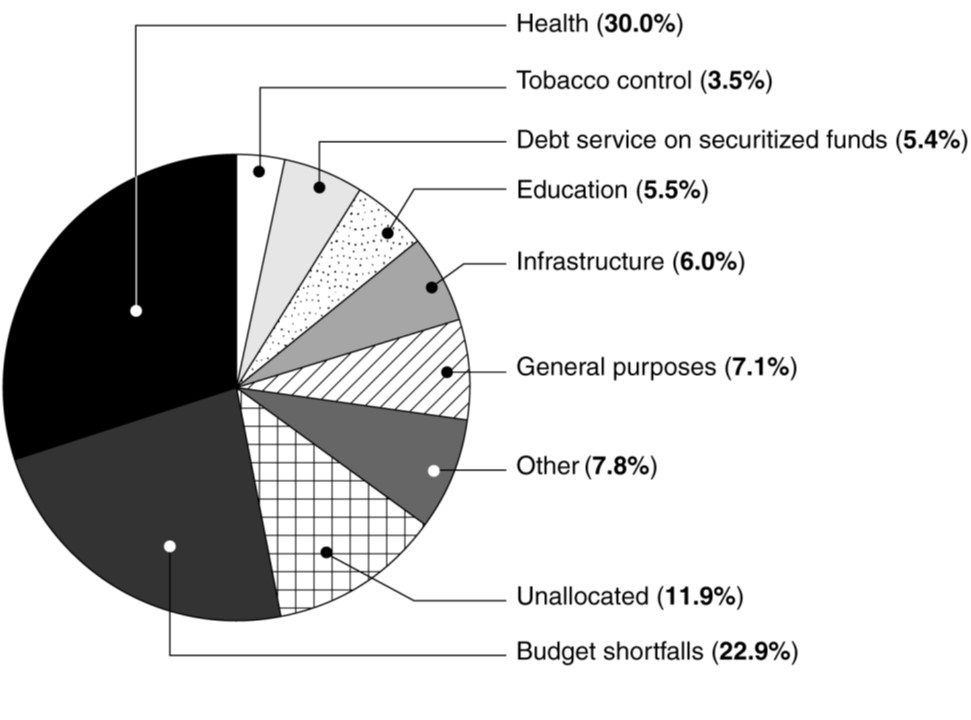
Figure 1. GAO analysis of categories to which states allocated their Tobacco Settlement payments (fiscal years 2000-2005) (3).
Another 7.1 percent had been spent on “general purposes” and another 6 percent on the politically popular term “infrastructure.” Other notable highlights were that 11.9 percent of funds were “unallocated” and 7.8 percent had been devoted to “Other.” Only about a third of the settlement revenues had been spent on health and tobacco control.
Much the same is likely to happen with the generic drug manufacturers lawsuit. A settlement will be reached and go into state funds and be viewed as a cash cow by legislators enthusiastic to cut taxes and/or fund their own pet projects. It seems likely that only a small portion will be spent on the public who for years have suffered inflated drug prices. After the settlement the generic manufacturers will be free to conduct business and fix prices as before.
If we can learn from the Tobacco Settlement, interventions can be taken to ensure the money is spent appropriately. States attorney generals should not be allowed to settle the suit benefiting those who were not harmed by unscrupulous price fixing. The spending of any settlement money should be supervised by the courts and the money should go directly to the state departments of health, away from tampering by state legislators and others. The money should be used to supplement healthcare for those who need the financial assistance the most. Since market forces regulating generic drug prices have apparently been corrupted, generic drug companies will need to have prices in the future approved assuring fair competition. Lastly, as a condition of settlement, CEOs need to sign agreements that impose severe penalties on both them and their companies for price fixing in the future.
Richard A. Robbins, MD
Editor, SWJPCC
References
- Simmons-Duffin S. States sue drugmakers over alleged generic-price-fixing scheme. All Things Considered. NPR. May 13, 2019. Available at: https://www.npr.org/sections/health-shots/2019/05/13/722881642/states-sue-drugmakers-over-alleged-generic-price-fixing-scheme (accessed 5/14/19).
- Pramuk J. Senators probing EpiPen price hike received donations from Mylan PAC. CNBC. Aug 26, 2016. Available at: https://www.cnbc.com/2016/08/26/senators-probing-epipen-price-hike-received-donations-from-mylan-pac.html (accessed 5/14/19).
- GAO. States’ allocations of payments from tobacco companies for fiscal years 2000 through 2005. US Government publication GAO-07-534T. February 27, 2007. Available at: https://www.gao.gov/assets/120/115580.pdf (accessed 5/14/19).
Cite as: Robbins RA. What will happen with the generic drug companies’ lawsuit: Lessons from the Tobacco Settlement. Southwest J Pulm Crit Care. 2019;18(6):155-6. doi: https://doi.org/10.13175/swjpcc032-19 PDF