Getting the Best Care at the Lowest Price
 Tuesday, September 25, 2012 at 9:55AM
Tuesday, September 25, 2012 at 9:55AM “Computers make it easier to do a lot of things, but most of the things they make it easier to do don't need to be done.”- Andy Rooney
A recent report from the IOM Institute of Medicine (IOM) claims that $750 billion, or about 30% of healthcare expenditures is wasted each year (1). This attention-grabbing statistic is reminiscent of the oft-quoted figure of 44,000-98,000 deaths attributable to medical errors annually from the 2000 IOM report titled “To Err Is Human: Building a Safer Health System” (2). The IOM estimate of deaths was based on two studies that used the Harvard Medical Practice Study methodology (3-6). Nurses reviewed charts and using preset criteria cases referred charts to physicians who had undergone a short training course. The physicians judged whether the adverse event was due to a medical error and whether the error contributed to the patient’s death. The incidence of deaths from medical errors was double in New York compared to Utah and Colorado resulting in the IOM’s high and low estimate. I remember reading the studies and thinking that both had problems. The physician reviewers were often outside the specialty area involved (e.g., nonsurgeons reviewing surgical cases); the criteria for error and whether it contributed to death were not clearly defined; and the results were inconsistent (were physicians from New York really twice as negligent as those from Utah and Colorado?). My impression was that no one would believe these flawed studies. I was very wrong. The IOM report helped spark an ongoing campaign for patient safety resulting in a number of interventions. Most were focused on physicians, some were expensive, and to date, it is unclear whether they have improved outcomes or wasted resources.
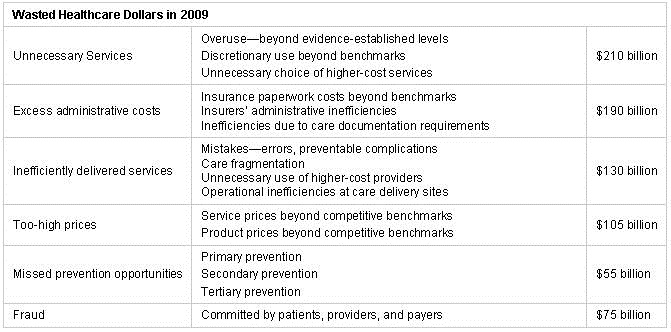
Now the IOM has published that an inefficient, extraordinarily complex, and slow-to-change US healthcare system wastes huge amounts of money (Table 1) (1).
Table 1. IOM estimates of wasted healthcare dollars.
Although the validity of the estimates is uncertain, most in healthcare would agree that a large portion of healthcare dollars are wasted. The report implies much of this inefficiency is due to clinicians because they are slow-to-change, inefficient and unable to keep up with the explosion in healthcare knowledge. Because of these limitations, physicians often mismanage the patient resulting in the waste of dollars noted above. In the healthcare system envisioned by the IOM, electronic health records (EHRs) would bring the research contained in more than 750,000 journal articles published each year to the point of care. Since it would be impossible for a clinician to read all 750,000 articles these would be communicated to the clinicians as guidelines.
Over the past decade, a remarkable number of laws, rules, regulations, and new ways of doing business have hit physicians (7). Each, when viewed alone, looks very reasonable, but, taken in aggregate, they are undermining the profession and medical care. Healthcare has become more expensive and physicians have shouldered this blame despite losing much of their autonomy. The IOM recommendations on computers may be another in the death by a thousand cuts that independently thinking physicians are receiving.
Although I’m resentful of the IOM report’s implications, bringing computers and EHRs to the clinic is a good idea. However, as a retired VA physician I have repeatedly heard how the “magic” of the computer can solve problems. The VA long ago installed an electronic health record with a set of guidelines that anyone could follow. Certainly improved efficiency and reduced costs would shortly follow. Unfortunately, this does not appear to be the case. When the VA EHR was instituted the numbers of physicians and nurses within the VA declined although the numbers of total employees increased (8). At least part of the increase was due to installation and maintenance of an EHR. At the same time an ever increasing number of guidelines were placed on the computer. Costs to ensure compliance and bonuses paid to administrators for compliance further escalated expenses. Furthermore, the guidelines caused a marked consumption of clinician time. According to one estimate, compliance with the source of many of the VA guidelines, the US Preventative Services Task Force, would require 4-7 hours of additional clinician time per day (9). Clearly, this was unsustainable so further money was allocated to hire healthcare technicians to comply with many of the guidelines. Compliance improved but efficiency, costs, morbidity or mortality did not (10). Furthermore, an unexpected increase in healthcare expenditures occurred outside the VA as a consequence of EHRs. A recent report from the Office of Inspector General of Health and Human Services notes an increase in higher level billing codes in Medicare patients (11). Experts say EHR technology resulted in the increase because of its super-charting capabilities (12). Therefore, it seems unlikely that EHRs as currently utilized will improve efficiency or lower costs.
Much to their credit, the IOM seems to recognize these limitations when they say, "Given such real-world impediments, initiatives that focus merely on incremental improvements and add to a clinician's daily workload are unlikely to succeed” (1). The report goes on to say that instead, the entire infrastructure and culture of healthcare must be reconfigured for significant change to occur. I would agree. Previous changes to improve healthcare have done nothing more than shift monies away from clinical care which will not improve patient outcomes (13). This occurred at the VA and will occur again if left unchecked. A meaningful partnership between clinicians and payers achieving and rewarding high-value care is needed. To do this physicians need considerable input, and perhaps more importantly, control of any EHR. Second, physicians need to be rewarded for good care which is centered on improved patient outcomes and not endless checklists that do little more than consume time. Failure to do so will result in inefficient and more costly care and not in the improvements promised by the IOM.
Richard A. Robbins, MD*
Editor, SWJPCC
References
- Smith M, Saunders R, Stuckhardt L, McGinnis JM. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academy Press. 2000. Available at: http://www.iom.edu/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America.aspx (accessed 9/8/12).
- Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building A Safer Health System. Washington, DC: National Academy Press. 2000. Available at: http://www.nap.edu/openbook.php?isbn=0309068371 (accessed 9/8/12).
- Hiatt HH, Barnes BA, Brennan TA, et al. A study of medical injury and medical malpractice. N Engl J Med 1989;321:480-4.
- Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med 1991;324:370-6.
- Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, Hebert L, Newhouse JP, Weiler PC, Hiatt H. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med 1991;324:377-84.
- Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, Howard KM, Weiler PC, Brennan TA. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 2000;38:261-71.
- Kellner KR. Physician killed by ducks. Chest 2005;127:695-6.
- Robbins RA. Profiles in medical courage: of mice, maggots and Steve Klotz. Southwest J Pulm Crit Care 2012;4:71-7.
- Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health 2003;93:635-41.
- Robbins RA, Gerkin R, Singarajah CU. Relationship between the Veterans Healthcare Administration hospital performance measures and outcomes. Southwest J Pulm Crit Care 2011;3:92-133.
- Office of Inspector General. Coding trends of Medicare evaluation and management services. Available at: http://oig.hhs.gov/oei/reports/oei-04-10-00180.asp (accessed 9-8-12).
- Lowes R. Are Physicians Coding Too Many 99214s? Medscape Medical News. Available at: http://www.medscape.com/viewarticle/767732 (accessed 9-8-12).
- Robbins RA, Gerkin R, Singarajah CU. Correlation between patient outcomes and clinical costs in the VA healthcare system. Southwest J Pulm Crit Care 2012;4:94-100.
*The views expressed in this editorial are those of the author and do not necessarily represent the views of the Arizona or New Mexico Thoracic Societies.
Reference as: Robbins RA. Getting the best care at the lowest price. Southwest J Pulm Crit Care 2012;5:145-8. (Click here for a PDF version of the editorial)

Reader Comments