May 2023 Critical Care Case of the Month: Not a Humerus Case
 Monday, May 1, 2023 at 8:00AM
Monday, May 1, 2023 at 8:00AM Billie Bixby2 MD
Janet Campion2 MD
Departments of Family and Community Medicine1 and Internal Medicine2
Banner University Medical Center-South Campus
Tucson, AZ USA
History of Present Illness:
A 57-year-old woman with history of bone disease presented with a 3-day history of cough with thick yellow phlegm and progressive shortness of breath. No fever, chest pain or abdominal pain was noted. In the emergency department, she had SpO2 of 55% on room air, and then 90% on 15L NRB.
Past Medical History/Social History/Family History
- Bone disease since birth
- Asthma
- Severe scoliosis
- Gastrointestinal reflux disease
- Cholecystectomy
- Spinal growth rods
- Lives in adult care home, supportive family
- No smoking or alcohol use
- No illicit drug use
- There is no family history of any bone disease
Home Medications:
- Albuterol MDI PRN
- Alendronate 10mg daily
- Budesonide nebulizer BID
- Calcium carbonate BID
- MVI daily
- Lisinopril 10mg daily
- Loratadine 10mg daily
- Metformin 500mg BID
- Metoprolol 12.5mg BID
- Montelukast 10mg daily
- Naprosyn PRN
- Omeprazole 20mg daily
- Simvastatin 10mg daily
- Tizanidine PRN
- Vitamin D 2000 IU daily
Allergies:
- Cefazolin, PCN, Sulfa - all cause anaphylaxis
Physical Examination :
- Vital signs: BP 135/95, HR 108, RR 36, Temp 37.0 C Noted to desaturate to SpO2 in 70-80s off of Bipap even when on Vapotherm HFNC
- General: Alert, slightly anxious woman, tachypneic, able to answer questions
- Skin: No rashes, warm and dry
- HEENT: No scleral icterus, dry oral mucosa, normal conjunctiva
- Neck: No elevated JVP or LAD, short length
- Pulmonary: Diminished breath sounds at bases, no wheezes or crackles
- Cardiovascular: Tachycardic, regular rhythm without murmur
- Abdomen: Soft nontender, nondistended, active bowel sounds
- Extremities: Congenital short upper and lower limb deformities
- Neurologic: Oriented, fully able to make health care decisions with family at bedside
Laboratory Evaluation:
- Na 142, K 4.3, CL 100, CO2 29, BUN 15, Cr 0.38, Glu 222
- WBC 21.9, Hgb 13.6, Hct 42.9, Plt 313 with 83% N, 8% L, 1% E
- Normal LFTs
- Lactic acid 2.2
- Venous Blood Gases (peripheral) on Bipap 10/5, FiO2 90%: pH 7.36, pCO2 58, pO2 55
- COVID-19 positive
Radiologic Evaluation:
A thoracic CT scan was performed (Figure 1).
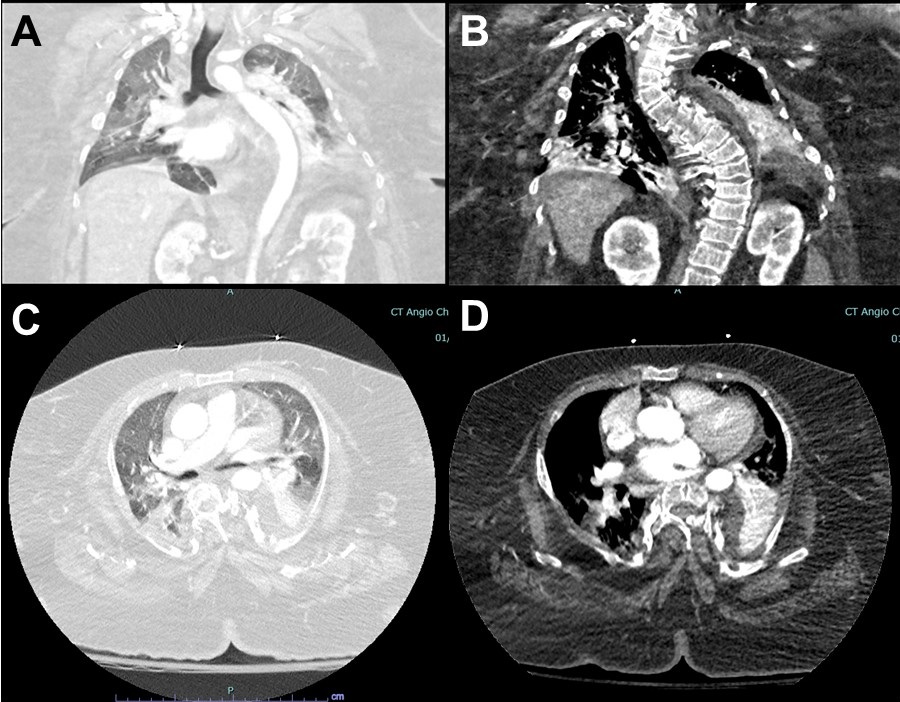 Figure 1. Representative images from thoracic CT scan in lung windows (A,C) and soft tissue windows (B,D).
Figure 1. Representative images from thoracic CT scan in lung windows (A,C) and soft tissue windows (B,D).
The CT images show all the following except: (Click on the correct answer to be directed to the second of seven pages)
- Severe scoliosis
- Diffuse ground glass opacities
- Right lower lobe consolidation
- Pneumothorax
- Atelectasis in bilateral lower lobes

Reader Comments