Essentials of Airway Management: The Best Tools and Positioning for First-Attempt Intubation Success
 Wednesday, April 19, 2023 at 8:00AM
Wednesday, April 19, 2023 at 8:00AM Evan D. Schmitz MD
Pulmonary and Critical Care Medicine
Abstract
Head position during endotracheal intubation affects first-attempt success, as does the different tools available and the location. It is important to be skilled in the operation of a variety of laryngoscopes (video or direct) as well as introducers (plastic/steel stylets and bougies). Difficult airways should always be anticipated and proper preparation such as upper airway assessment performed. The following is a review of endotracheal intubations performed outside of the operating room.
Objectives
- Discuss how different locations in the hospital can affect endotracheal intubation success.
- Learn the difference between simple head positioning and the sniffing position and why one should be chosen over the other. MRI images of the head and neck in each position will be reviewed.
- Learn about different types of laryngoscope blades.
- Understand the dangers of video laryngoscopy as well as the benefits and when to choose direct laryngoscopy.
- Define endotracheal intubation first-attempt success.
- The benefits of using a bougie as opposed to a stylet to increase first-attempt success rate with a review of the supportive literature.
- Case presentations.
Abbreviations
- AF – atrial fibrillation
- ARDS – acute respiratory distress syndrome
- BiPAP – bilevel positive airway pressure
- CAD – coronary artery disease
- COPD – chronic obstructive pulmonary disease
- Ó – delta
- DM – diabetes mellitus
- DVT – deep vein thrombosis
- ED – emergency department
- ETT – endotracheal tube
- FiO2 – fraction of inspired oxygen
- HFNC – high flow nasal canula
- HTN – hypertension
- ICU – intensive care unit
- LA – laryngeal axis
- LV – line of vision
- MRI – magnetic resonance imaging
- NIDDM – non-insulin dependent diabetes mellitus
- NRB – non-rebreather mask
- OA – oral axis
- OR – operating room
- OSA – obstructive sleep apnea
- PA – pharyngeal axis
- PCO2 – partial pressure of carbon dioxide
- PE – pulmonary embolism
- RCA – right coronary artery
- SpO2 – pulse oximeter oxygen saturation
- Sz – seizure
Introduction
Ideal positioning can make the difference between a successful endotracheal intubation or death. Many times, intubations are performed in emergency situations, and positioning is not always ideal depending on the type of surface. In the OR, ideal conditions exist regarding adequate supplies and time (1). Conditions can be very different outside of the operating room (OR) especially during a code blue. The average time of intubation is 37 seconds in the emergency department (ED) (2). During the COVID-19 pandemic, intubations were being performed as quickly as 15 seconds in the intensive care unit (ICU) to prevent cardiac arrest in patients with severe adult respiratory distress syndrome (ARDS) (3).
Hospital beds are cumbersome and can cause poor positioning making intubation difficult. If possible, it is always a good idea to have a few towels available to help with head positioning. Towels can be rolled up and placed between the shoulder blades to aid in simple head extension. Towels can also be used to flex the neck on the chest and extend the head on the neck into the sniffing position. Pillows can be added if needed in morbidly obese patients.
Previous studies published in the Journal of Anesthesia comparing head positioning with regards to line of vision (LV), oral axis (OA), pharyngeal axis (PA), and laryngeal axis (LA) proved that all axes can never be perfectly aligned (Figure 1) (4). The same authors concluded that routine use of the sniffing position appears to provide no significant advantage over simple head extension for tracheal intubation (5).
The sniffing position improved glottic exposure in 18% of patients and worsened it in 11% in comparison with simple head extension in patients intubated in the operating room. Multivariant analysis showed that patients with reduced neck mobility and obesity did better in the sniffing position.
The angle between the LV to the LA, ó, decreases significantly when placed in simple head extension (B) and the sniffing position (C) compared with neutral positioning (A) (Figure 1). In simple head extension ó is the smallest approximating 20o. The smaller the ó, the easier it is to access the glottis. Bougie introducers like the AIROD® telescopic steel bougie with a 20o bend at the proximal end as well as elastic bougies with a coude (bent) tip allow easy transition from the LV to the laryngeal axis LA in simple head extension Figure 2 (6-10).
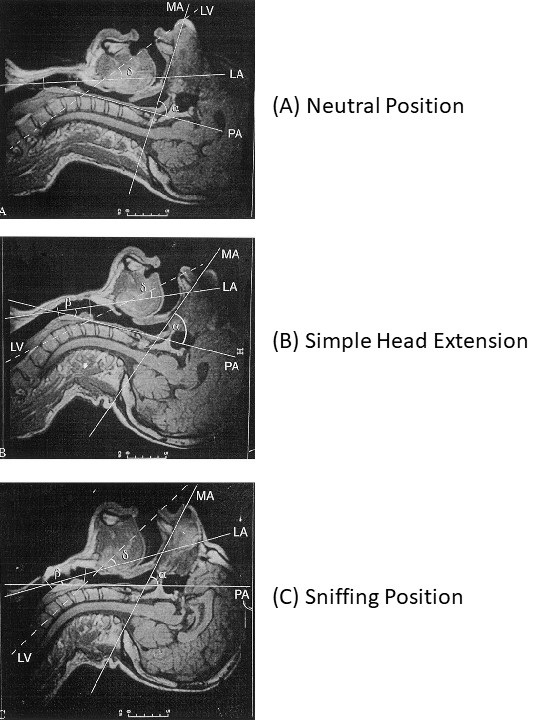 Figure 1. Evaluation of the four axes (mouth axis [MA], pharyngeal axis [PA], laryngeal axis [LA], line of vision [LV] and the α, β, and ό angles in the three positions (4).
Figure 1. Evaluation of the four axes (mouth axis [MA], pharyngeal axis [PA], laryngeal axis [LA], line of vision [LV] and the α, β, and ό angles in the three positions (4).
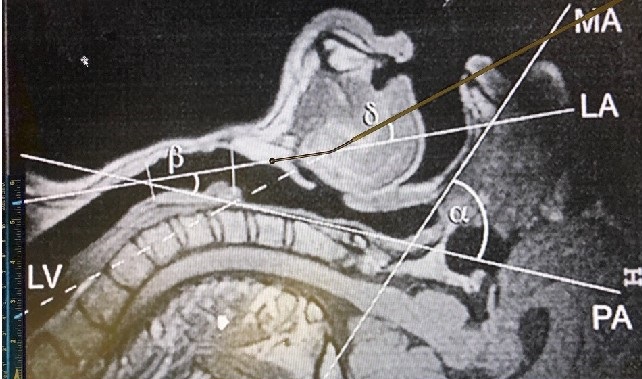 Figure 2. AIROD® aligned perfectly with the laryngeal view (LV) with the head in simple extension. Transition to the laryngeal axis (LA) is easy due to the specialized 20o tip.
Figure 2. AIROD® aligned perfectly with the laryngeal view (LV) with the head in simple extension. Transition to the laryngeal axis (LA) is easy due to the specialized 20o tip.
The different video laryngoscopes all offer indirect views of the glottis (Figure 3).
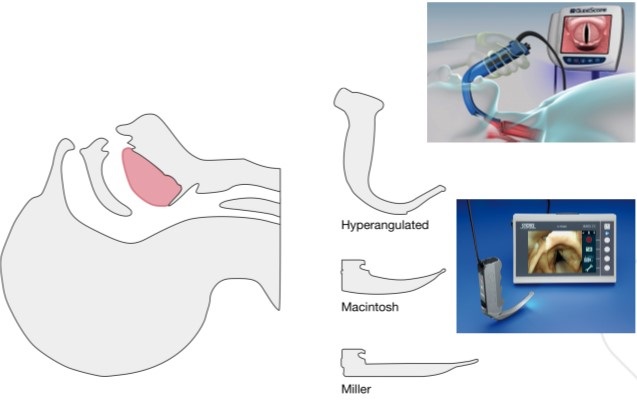
Figure 3. Different types of video and direct laryngoscopes.
For those on C-spine precautions, a hyperangulated Glidescope® or C-MAC® can help with the acute angles involved without the need for significant neck movement. Although video laryngoscopes may improve the view of the glottis because they do not guarantee a direct pathway to the vocal cords, disaster may occur during intubation. Additional tools and expertise should be available immediately because once sedatives and paralytics are given you may no longer be able to ventilate the patient.
In 2017 Baptiste et al. (11) published a study showing that severe life-threatening complications were higher in those ICU patients who were intubated using video laryngoscopy 9.5% vs 2.8% in those who were intubated with direct laryngoscopy with the numbers needed to harm of 14.6. Blood, emesis, secretions, damaged screen, and sudden battery failure can all obscure the video images, complicating intubation with video devices. It is therefore recommended that operators be comfortable using direct laryngoscopes as well as bougies in case of video device failures.
Prior to intubation, airway assessment should be performed to determine whether a difficult airway may be present. If any of the following characteristics are present, then a difficult airway should be expected and precautions taken:
- Mouth opening < 3.5 cm
- Thyromental distance < 6.5 cm
- BMI > 30 kg/m2
- Amplitude of head and neck movement < 80o
- Mallampati score > 3
- Cormack and Lehane classification > 2
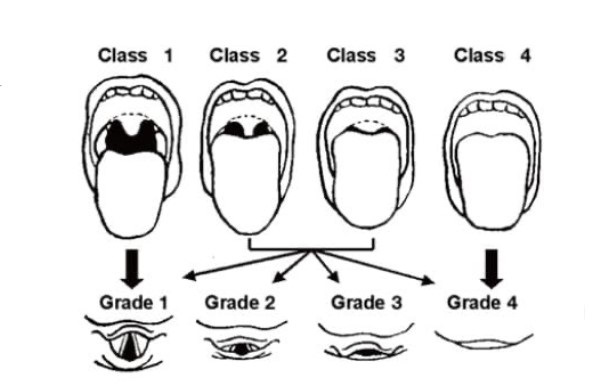 Figure 4. Mallampati scores classes 1-4 and Cormack and Lehane classification grades 1-4.
Figure 4. Mallampati scores classes 1-4 and Cormack and Lehane classification grades 1-4.
In addition to these measurements, a difficult airway is present if the airway is obstructed by emesis, blood, foreign object or swelling; if the patient has a short neck, large tongue, facial trauma; or if cervical spine immobilization is needed.
Increased complications arise during intubation when a difficult airway is present, especially in an unstable patient. Adverse events related to endotracheal intubation in the ED have been reported at 12% (11). Only 70% of patients intubated in the ICU are successfully intubated upon first-attempt (12). A successful first-attempt intubation is defined as the placement of an endotracheal tube into the trachea upon the initial insertion of the laryngoscope into the oropharynx. If the laryngoscope must be removed and a second-attempt performed, it is considered a failure. Failure to intubate with the first-attempt contributes considerably to morbidity and mortality (13).
The choice of the correct endotracheal introducer can make the difference between first-pass success and failure (Figure 5).
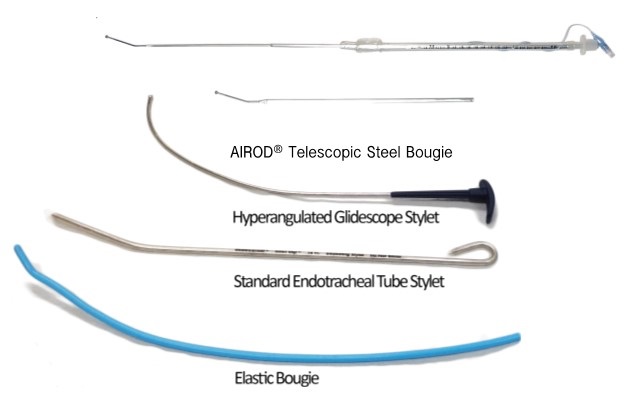 Figure 5. Types of airway introducers.
Figure 5. Types of airway introducers.
The standard endotracheal tube stylet is used most often during direct laryngoscopy. This stylet may be bent when used with a curved Macintosh blade or without a bend when used with a straight Miller blade. The former is the most common method. An elastic bougie has an advantage over the standard stylet as it can be placed through the vocal cords and into the trachea, allowing better access especially with anterior airways during direct laryngoscopy with a Macintosh or Miller blade.
The BEAM (Bougie Use in Emergency Airway Management) trial is attracting renewed interest in intubation with a bougie rather than a stylet (2). In the BEAM trial, first-attempt success using an elastic bougie was compared to a stylet during laryngoscopy in an emergency department.
First-attempt success was achieved in 98% of patients compared to 87% in all patients. In patients with at least one difficult airway characteristic, first-attempt success using an elastic bougie was 96% compared to 82% using a stylet.
In the First-Attempt Endotracheal Intubation Success Rate Using a Telescoping Steel Bougie (3), intubation first-attempt success rate was 97% in the ICU. Subgroup analysis of first-attempt intubation success using the AIROD® to intubate in patients with a difficult airway was 96%.
The average time to intubate was 15 seconds. During multiple intubations, the AIROD® was used to lift the epiglottis and move excess oropharyngeal tissue, improving the view of the glottis without causing any trauma to the airway (Figure 6).
 Figure 6. Video of AIROD® lifting the epiglottis.
Figure 6. Video of AIROD® lifting the epiglottis.
The hyperangulated Glidescope® stylet can be used with the Glidescope®, curved Macintosh blade, and C-MAC® blade. The AIROD® can be used with any direct or video laryngoscopy in any configuration: curved, hyperangulated, or straight.
The elastic bougie cannot make the acute turn required with hyperangluated laryngoscopes and should be avoided with this device unless the hyperangulated Glidescope® stylet is placed first and becomes caught up on the superior angle of the vocal cords. If this occurs, leave the Glidescope® in position and gently remove the hyperangulated Glidescope® stylet. While maintaining the acute angle, introduce an elastic bougie into the ETT and advance the tip into the trachea. Then slide the ETT down the bougie and into the trachea.
An alternative is to use the AIROD® steel bougie from the beginning, along with the Glidescope®. Load an ETT from the bulbous tip of the AIROD®, then shape to accommodate airway anatomy (Figures 7 and 8).
 Figure 7. AIROD® shaped to accommodate airway anatomy.
Figure 7. AIROD® shaped to accommodate airway anatomy.
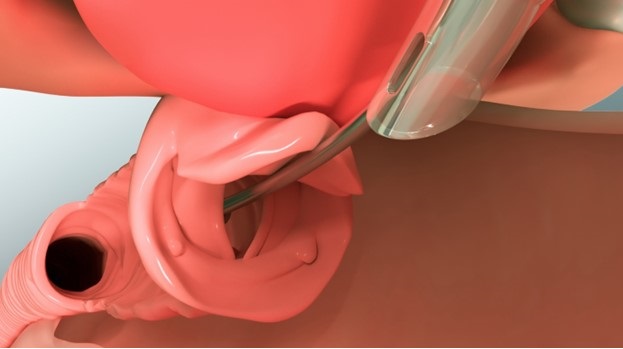 Figure 8. ETT advancing down the AIROD®.
Figure 8. ETT advancing down the AIROD®.
Use the proximal tip to lift the epiglottis and expose the vocal cords. Then advance the AIROD® two cm into the trachea followed by the ETT.
Case Presentations
Case 1
54-year-old man with severe coronary artery disease on aspirin and Plavix® with a history of a seizures associated with alcohol withdrawal became unresponsive and a code blue was called. He was found to be apneic with oxygen saturation in the 50s. He was stimulated by the hospitalist and became responsive. He was transferred to the ICU, where he became completely unresponsive again and stopped breathing. He was immediately ventilated with a bag-valve mask, and oxygenation improved to 100%. He then bolted up out of bed and became very combative. Propofol was given and he was laid supine and ventilated with a bag-valve mask. Inspection of his oropharynx revealed a very large tongue, and some missing and multiple sharp teeth with mouth opening of only 2 fingerbreadths. There was blood and emesis in his oropharynx that was suctioned. A Miller 4 blade was inserted into the oropharynx but only a grade 4 view could be obtained. The AIROD® was inserted into the oropharynx in the fully extended and locked position and the proximal tip was used to gently lift the epiglottis, exposing the vocal cords, and improving the view to a grade 2. The AIROD® was advanced 2 cm past the vocal cords and an assistant advanced an 8.0 endotracheal tube down the AIROD® until it was grasped, and the endotracheal tube was advanced successfully past the vocal cords while the assistant held the distal end of the AIROD®. The AIROD® was removed intact without any oropharyngeal or vocal cord trauma.
Case 2
A 63-year-old 5’5 110 kg woman with COPD, morbid obesity, obstructive sleep apnea, atrial fibrillation, diabetes mellitus, and anxiety suffered a cardiac arrest and was successfully resuscitated with placement of a drug eluting stent into the right coronary artery. One week later she required intubation for acute respiratory failure. She was extubated the following day and developed stridor, which resolved with pain medication and racemic epinephrine. Two days later, she developed acute respiratory failure again, with stridor that resolved after receiving 4 mg IV Versed. A diagnosis of paroxysmal vocal cord dysfunction was made. The next day she developed similar symptoms that responded to additional Versed® and Precedex®. The next morning, she became anxious after the Precedex® was stopped and once again developed acute stridor with respiratory failure, responding to Zyprexa® and Versed® momentarily. She was comfortable throughout the day until her stridor resumed, and despite BiPAP she was unable to adequately ventilate. She became obtunded, prompting intubation.
In addition to stridor, her Mallampati was 4, she had a sharp, prominent full set of teeth, an airway opening 1.5 cm, a large tongue with excessive oropharyngeal tissue, false cords, and vocal cord swelling. The AIROD® was preloaded with a 7.0 ETT that had attached to it a 10 mL syringe onto the distal end and tucked it under the patient’s right shoulder with the tip lying flat and pointing laterally, protected with a sterile OR towel. The AIROD® lay at a 45o to the neck. She was given 20 mg of etomidate and immediately ventilated with a bag-valve mask. A Miller 4 blade was gently inserted into the mouth, revealing a grade 4 view with purulent mucus in her oropharynx. The AIROD® was grasped and used to manipulate the false cords, revealing the true vocal cords while cricoid pressure was applied. A grade 2 view was obtained. The cords were adducted with a posterior glottal chink. The AIROD® was gently passed 2 cm through the tiny opening at the bottom of the vocal cords and used to dilate the area with the smooth bulbous tip. The ETT was then advanced into the trachea while the respiratory therapist held the distal end of the AIROD®. The AIROD® was removed intact without any evidence of oropharyngeal trauma. Successful first-attempt intubation occurred without complications. Bronchoscopy confirmed no tracheobronchial tree trauma.
Case 3
A 71-year-old 5’10’’ tall 101 kg man with non-insulin dependent diabetes mellitus, hypertension, and obesity was intubated 18 days prior for severe ARDS secondary to SARS-CoV-2. He subsequently lost his airway, and the attending physician was unable to intubate using the Glidescope®; so an emergency tracheostomy was performed with placement of a 5.0 Shiley. The evening of the 24th day of ventilation, he was unable to be ventilated effectively with his PCO2 rising to 73 mmHg with a pH of 7.13. He was on a propofol drip and 10 mg vecuronium was given while he was being ventilated through the 5.0 tracheostomy. He was actively bleeding from his nasopharynx. A Miller 4 blade was gently inserted into his mouth revealing a bloody and swollen oropharynx. A pre-loaded AIROD® was used to gently displace tissue, revealing a grade 1 view. The AIROD® was inserted 1 cm past the vocal cords and the ETT was then advanced slowly into the trachea with no assistant holding the AIROD®. The AIROD® was pulled back as the endotracheal tube was advanced down the trachea, abutting the tracheostomy tube. The ETT balloon was inflated and the AIROD® was removed intact without any evidence of acute oropharyngeal trauma. The single-handed first-attempt intubation was performed in 19 seconds. This was followed by the exchange of the 5.0 tracheostomy for an 8.0 tracheostomy. Bronchoscopy confirmed no acute oropharyngeal or tracheal trauma with the tracheostomy in the correct position in the trachea.
Case 4
A 68-year-old 5’10 126 kg smoker with a past medical history significant for COPD, on home oxygen with multiple intubations in the past was admitted. He had a past medical history of pulmonary embolism on Eliquis®, deep venous thrombosis with an inferior vena cava filter, obstructive sleep apnea, and obesity. He was diagnosed with COVID-19 pneumonia and treated with BiPAP at 100% FiO2 for six days in the ICU. He developed ARDS and altered mental status, prompting intubation. Obese, large neck with limited neck mobility, micrognathia, large very dry tongue, sharp teeth with some missing, and a mouth opening 2 cm. He received propofol 200 mg IV and succinylcholine 200 mg IV. A Miller 4 blade gently inserted into oropharynx revealed an anterior glottis with false cords. The AIROD® was used to probe the false cords and advanced gently 5 cm, feeling the tracheal rings to ensure placement in the trachea. An 8.0 ETT was slowly advanced into the trachea using the single-handed first-attempt technique. An endotracheal balloon was inflated and the AIROD® removed intact without any evidence of acute oropharyngeal or tracheal trauma.
Case 5
28-year-old 5’9 man 97 kg with a past medical history significant for alcoholism was admitted. He was currently drinking two liters of vodka daily, had a history of alcoholic cardiomyopathy and esophageal varices, drank hand sanitizer “to remain drunk”, and developed acute shortness of breath, and felt that his “throat was closing”. He developed very severe stridor with respiratory distress and was transferred to the ICU. Audible stridor could be heard as he arrived. He was in severe respiratory failure, sitting up, and very anxious. He was drooling bloody secretions. He was placed on a 15 L/min 100% FiO2 non-rebreathing mask. He was obese, had a large large neck with limited mobility, mouth opening 2 cm, protruding large tongue, full set of teeth, micrognathia with severe stridor, and was barely moving any air. He was given 4 mg IV Versed®. A tracheostomy kit was at bedside with a surgeon present. He was given 100 mg IV propofol, then laid flat and quickly placed in the SNIFF position. Bag-valve-mask was performed. SpO2 100%. An additional 100 mg IV propofol was given. A Miller 4 blade barely lifted the tongue when fresh blood was encountered. The blade was advanced gently, and bloody secretions suctioned. A crowded anterior hamburger oropharynx, bleeding with mucosal sloughing and false cords was encountered. The AIROD® pre-loaded with a 6.5 ETT was gently advanced underneath the epiglottis and advanced 3 cm, followed by advancement of the 6.5 ETT. Bag-valve ventilation occurred with poor CO2 detector color change. The ETT was left in place while bag-valve-mask ventilation was performed. SpO2 100%. The AIROD® was pre-loaded with a 7.0 ETT. A second-attempt revealed an air bubble anterior to the ETT. The 6.5 ETT was removed as the AIROD® was advanced towards the air bubble. The AIROD® was used to probe the hamburger glottis and to peel back the false cords revealing a small view of the right vocal cords, followed by advancement of the AIROD® 3 cm. A 7.0 ETT was slowly advanced into the trachea and balloon inflated with no assistant holding the AIROD®. No evidence of acute oropharyngeal trauma. Bronchoscopy revealed no tracheobronchial trauma and confirmed acute adenoviral necrotizing pharyngitis.
Conclusion
Anticipation of a difficult airway should always be considered, and having the necessary tools available can improve first-attempt endotracheal intubation success. Optimizing head positioning can be performed quickly and will help with glottic exposure. Knowing how to use multiple laryngoscopes as well as introducers can make the difference between life and death.
Conflicts of Interest
Evan D. Schmitz, MD is the inventor of the AIROD® and CEO of AIROD Medical, LLC.
Acknowledgments
The author thanks H. Carole Schmitz and Bille J. Maciunas for their editorial comments.
References
- Sasano N, Morita M, Sugiura T, Sasano H, Tsuda T, Katsuya H. Time progression from the patient's operating room entrance to incision: factors affecting anesthetic setup and surgical preparation times. J Anesth. 2009;23(2):230-4. [CrossRef] [PubMed]
- Driver B, Prekkar M, Klein L, et al. Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation a randomized clinical trial. JAMA. 2018;319(21):2179-2189. [CrossRef] [PubMed]
- Schmitz ED. Decreasing COVID-19 patient risk and improving operator safety with the AIROD during endotracheal intubation. J of Emergency Services. EMSAirway. 11/2020.
- Adnet F, Borron SW, Dumas JL, Lapostolle F, Cupa M, Lapandry C. Study of the "sniffing position" by magnetic resonance imaging. Anesthesiology. 2001 Jan;94(1):83-6.[CrossRef] [PubMed]
- Adnet F, Baillard C, Borron SW, et al. Randomized study comparing the "sniffing position" with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiology. 2001 Oct;95(4):836-41. [CrossRef] [PubMed]
- Schmitz ED, Park K. First-Attempt Endotracheal Intubation Success Rate Using A Telescoping Steel Bougie. Southwest J Pulm Crit Care. 2021;22(1):36-40. doi: [CrossRef]
- Schmitz ED, Park K. Emergency intubation of a critically ill patient with a difficult airway and avoidance of cricothyrotomy using the AIROD®. J of Emergency Medical Services. 2021;22(1):36-40.
- Schmitz ED. Single-use telescopic bougie: case series. Southwest J Pulm Crit Care. 2020;20(2):64-8. [CrossRef]
- Schmitz ED. AIROD® Case Series: A New Bougie for Endotracheal Intubation. J of Emergency and Trauma Care. 2020;5(2):22.
- Schmitz ED. The Importance of Head Positioning During Endotracheal Intubation. EMSAirway. Jul 27, 2021. Available at: https://emsairway.com/2021/07/27/the-importance-of-head-positioning-during-endotracheal-intubation/#gref (accessed 4/18/23).
- Lascarrou JB, Boisrame-Helms J, et al. Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU Patients: A Randomized Clinical Trial. JAMA. 2017;317(5):483-493. [CrossRef] [PubMed]
- Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, Cook TM; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; Royal College of Anaesthetists. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018 Feb;120(2):323-352. [CrossRef] [PubMed]
- Brown CA 3rd, Bair AE, Pallin DJ, Walls RM; NEAR III Investigators. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med. 2015 Apr;65(4):363-370.e1. [CrossRef] [PubMed]

Reader Comments (2)
This is clear propaganda, has this journal turned into advertising space?
In response to Shameful, the journal relies upon reviewers to identify potential conflicts of interest. A conflict of interest statement was at the bottom of the article. Neither of two reviewers commented on "propaganda" nor identified any conflicts that they felt were sufficient to preclude publication.
Richard A. Robbins MD
Editor, SWJPCCS