Medical Image of the Week: Bochdalek Hernia
 Wednesday, June 1, 2016 at 8:00AM
Wednesday, June 1, 2016 at 8:00AM 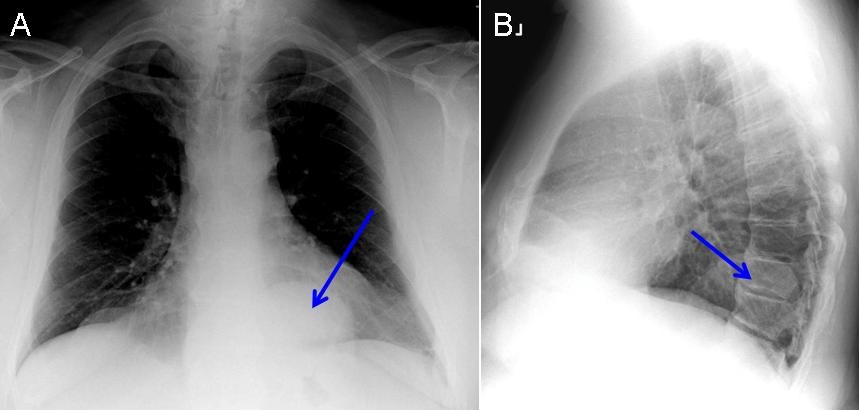
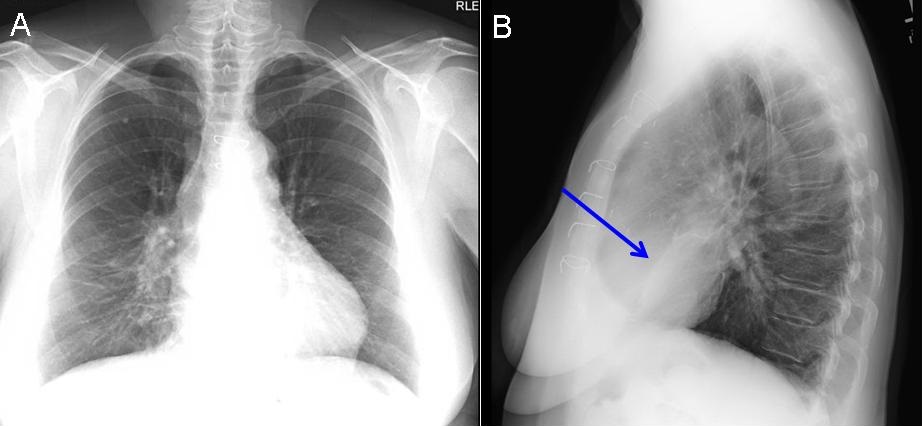
Figure 1. PA (A) and lateral (B) chest radiograph demonstrating a lobulated homogenous opacity in the posterior left lung base-blue arrows.
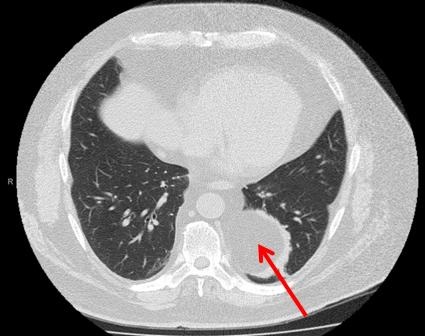
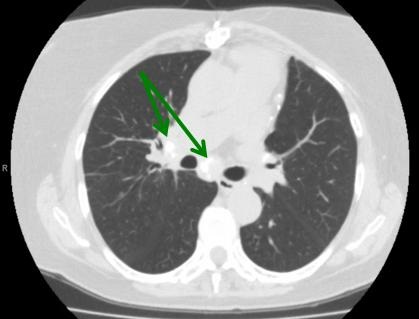
Figure 2. Chest CT (axial image) demonstrating fat-containing opacity consistent with a Bochdalek hernia- red arrow.
A 61 year-old man presented for an evaluation of a nonproductive cough. He has a history of well-controlled asthma, allergic rhinitis and nasal polyposis, hypertension, gastro-esophageal reflux and obstructive sleep apnea. The ACE inhibitor used to treat hypertension was discontinued. The physical exam was unremarkable. Pulmonary function testing was normal.
A PA and lateral chest radiograph was performed and revealed an abnormal contour of the left hemidiaphragm with a large lobulated opacity (Figure 1- blue arrows). Computed chest tomography revealed the lobulated opacity in the left lower lobe contained fat and was consistent with a Bochdalek hernia (Figure 2).
Congenital diaphragmatic hernia is a major malformation in newborns and in the perinatal period. The diagnosis of congenital diaphragmatic hernia in adults is rare. There are three types of congenital diaphragmatic hernias: posterolateral (Bochdalek) diaphragmatic hernia, subcostosternal (Morgagni) hernia and esophageal hiatal hernia. The Bochdalek diaphragmatic hernia is the result of a congenital diaphragmatic defect in the posterior costal part of the diaphragm in the region of 10th and 11th ribs, which allows free communication between the thoracic and abdominal cavity. The defect is usually found at the left side (90%) but may occur on the right side, where the liver often prevents detection.
A review of 173 adult patients with Bochdalek hernias revealed several important features: 55% of patients were male with an average age of 40 years, the hernia defect was located on the left side in 78% of patients and most patients were symptomatic (1,2). The most common presenting symptoms were pain or pressure in the chest or abdomen and obstruction. Pulmonary symptoms occurred in 37% of patients in this review. Of note, patients with Bochdalek hernias can develop symptoms precipitated by factors that increase intra-abdominal pressure and failure to promptly treat a symptomatic Bochdalek hernia may lead to bowel strangulation. A chest CT is an excellent diagnostic study, as a Bochdalek hernia can be difficult to appreciate on a chest radiograph (3).
Management of a Bochdalek hernia includes reducing the abdominal contents and repairing the defect through a laparotomy or thoracotomy. Successful laparoscopic and thoracoscopic repairs of Bochdalek hernias have both been described.
Muna Omar, M.D. and Linda Snyder, M.D.
Pulmonary, Critical Care, Sleep and Allergy Medicine
Banner University Medical Center-Tucson
Tucson, AZ USA
References
- Brown SR, Horton JD, Trivette E, Hofmann LJ, Johnson JM. Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia. 2011 Feb;15(1):23-30. [CrossRef] [PubMed]
- Bianchi E, Mancini P, De Vito S, Pompili E, Taurone S, Guerrisi I, Guerrisi A, D'Andrea V, Cantisani V, Artico M. Congenital asymptomatic diaphragmatic hernias in adults: a case series. J Med Case Rep. 2013 May 13;7:125. [CrossRef] [PubMed]
- Sandstrom CK, Stern EJ. Diaphragmatic hernias: a spectrum of radiographic appearances. Curr Probl Diagn Radiol. 2011 May-Jun;40(3):95-115. [CrossRef] [PubMed]
Cite as: Omar M, Snyder L. Medical image of the week: Bochdalek hernia. Southwest J Pulm Crit Care. 2016 Jun;12(6):203-4. doi: http://dx.doi.org/10.13175/swjpcc031-16 PDF