Medical Image of the Week: Complex Arteriovenous Malformation
 Wednesday, May 18, 2016 at 8:00AM
Wednesday, May 18, 2016 at 8:00AM 
Figure 1. Initial chest radiograph demonstrating right mid lung field process.

Figure 2. Panel A: Contrast enhanced thoracic CT scan axial view demonstrating very large, complex AVM. Panel B: Sagittal view.

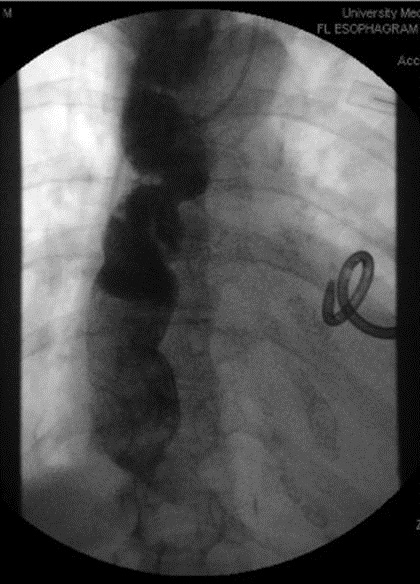
Figure 3. Chest radiograph after coil embolization.
A 62-year-old man presented to the emergency department complaining of shortness of breath with exertion and mild non-productive cough. The patient was afebrile and physical exam was remarkable only for scattered bilateral rhonchi. White blood cell count was 8,800 K/uL and hematocrit was 51.5%. Room air arterial blood gas (at 1520 meters altitude) was pH 7.41, pCO2 42 mm Hg, PO2 45 mm Hg, and O2 saturation 78%. D-dimer was normal at 0.36 ug/ml. Chest radiograph (Figure 1) demonstrated what was interpreted as a right-sided mid/lower lung field infiltrate. The patient was placed on high-flow supplemental oxygen and treatment was initiated with intravenous levofloxacin, methylprednisilone and nebulized beta-agonists. The patient’s oxygenation failed to improve over a period of several days, and a CAT of the chest (Figures 2) was obtained, which demonstrated a very large, right middle lobe, complex pulmonary arteriovenous malformation. The patient was referred to interventional radiology for catheter directed coil embolization (Figure 3). Following that procedure the patient’s oxygen requirement decreased from 15 l/m via nasal cannula to 3 l/m.
Pulmonary arteriovenous malformations (PAVM’s) are rare, with an incidence of 2-3 per 100,000, and are associated with hereditary hemorrhagic telangiectasia (HHT), in approximately 80% of cases (1). The intrapulmonary shunt associated with PAVM’s may result in significant hypoxemia, cerebrovascular accident or embolic brain abscess. The preferred screening tool is transthoracic contrast echocardiography, which demonstrates extra-cardiac shunt. Chest CT scan may be used to both confirm the diagnosis of PAVM and to define the vascular anatomy. Patients who meet three of the four Curacao criteria (epistaxis, family history, telangiectasia, and visceral lesions) are recognized as suffering from HHT (2). Catheter directed coil embolization is an effective and well-tolerated treatment method for PAVM; and generally results in reduced shunt fraction and improved oxygenation (3).
Kathleen Monahan and Charles J. VanHook MD
Longmont United Hospital
Longmont, Colorado USA
References
- Cartin-Ceba R, Swanson KL, Krowka MJ. Pulmonary arteriovenous malformations. Chest. 2013 Sep;144(3):1033-44. [CrossRef] [PubMed]
- Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, Kjeldsen AD, Plauchu H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. 2000 Mar 6;91(1):66-7. [CrossRef] [PubMed]
- Dutton JA, Jackson JE, Hughes JM, Whyte MK, Peters AM, Ussov W, Allison DJ.Pulmonary arteriovenous malformations: results of treatment with coil embolization in 53 patients. AJR Am J Roentgenol. 1995 Nov;165(5):1119-25. [CrossRef] [PubMed]
Cite as: Monahan K, VanHook CJ. Medical image of the week: complex arteriovenous malformation. Southwest J Pulm Crit Care. 2016 May;12(5):197-8. doi: http://dx.doi.org/10.13175/swjpcc027-16 PDF