Medical Image of the Week: Superior Vena Cava Syndrome
 Wednesday, August 31, 2016 at 8:00AM
Wednesday, August 31, 2016 at 8:00AM 
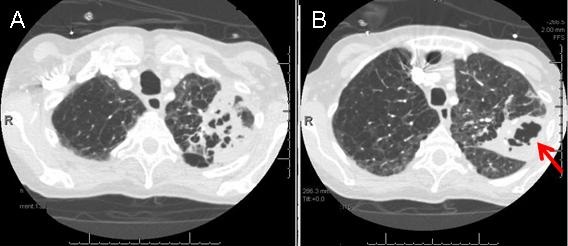
Figure 1. Thoracic CT in soft tissue windows. Panels A, B, C and G show extensive collateral circulation along the right chest wall especially subcutaneous vessels and subcapsular hepatic vessels during contrast injection in the right arm (arrows). There are also prominent right hepatic and capsular enhancing vessels with vascular shunt within the posterior subcapsular right hepatic lobe. Panels D, E, F and I show extensive collateral circulation on the left side when the contrast is injected (on a different admission) in the left arm (arrows). Panel H shows absent blood flow in the totally thrombosed SVC stent.
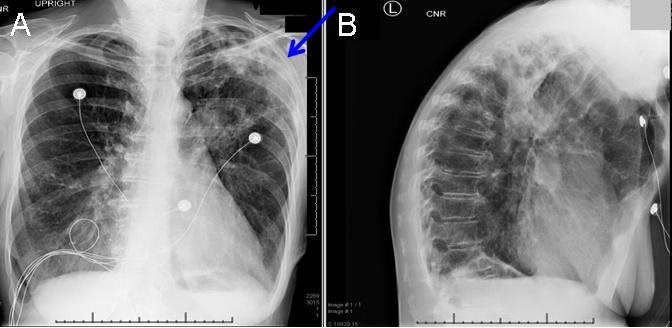
Superior vena cava (SVC) syndrome results from obstruction of blood flow in the SVC. Most cases are secondary to malignancy, the most common being lung cancer or non-Hodgkin lymphoma. Other less encountered etiologies include fibrosing mediastinitis and thrombosis associated with intravascular devices (1,2). Here, we present a case of advanced lung cancer undergoing chemo-radiation therapy who presented with typical symptoms of SVC syndrome including progressive shortness of breath and facial swelling/ fullness over weeks to months. His chest CT scan showed SVC obstruction due to his tumor mass (Figure 1). The patient underwent stenting and improved partially for sometime. However, he returned again with worsening symptoms over a few weeks with discovery of SVC in-stent thrombosis. He was started on therapeutic enoxaparin and his symptoms improved partially with time.
Huthayfa Ateeli, MBBS1, Kawanjit Sekhon, MD2 and Dena K. L'Heureux, MD3.
1Department of Medicine, Division of Pulmonary, Critical Care, Sleep and Allergy Medicine; 2Department of Medicine, Internal Medicine Residency Program, Main Campus; and 3Department of Medicine, Division of Pulmonary, Critical Care, Sleep and Allergy Medicine, University of Arizona, Southern Arizona VA Health Care System, Tucson, AZ USA
References
- Wilson LD, Detterbeck FC, Yahalom J. Clinical practice. Superior vena cava syndrome with malignant causes. N Engl J Med. 2007 May 3;356(18):1862-9. [CrossRef] [PubMed]
- Rice TW, Rodriguez RM, Light RW. The superior vena cava syndrome: clinical characteristics and evolving etiology. Medicine (Baltimore). 2006 Jan;85(1):37-42. [CrossRef] [PubMed]
Cite as: Ateeli H, Sekhon K, L'Heureux DK. Medical image of the week: superior vena cava syndrome. Southwest J Pulm Crit Care. 2016;13(2):99-100. doi: http://dx.doi.org/10.13175/swjpcc065-16 PDF