Medical Image of the Week: PE with Infarct and Pulmonary Cavitation
 Wednesday, December 10, 2014 at 8:00AM
Wednesday, December 10, 2014 at 8:00AM 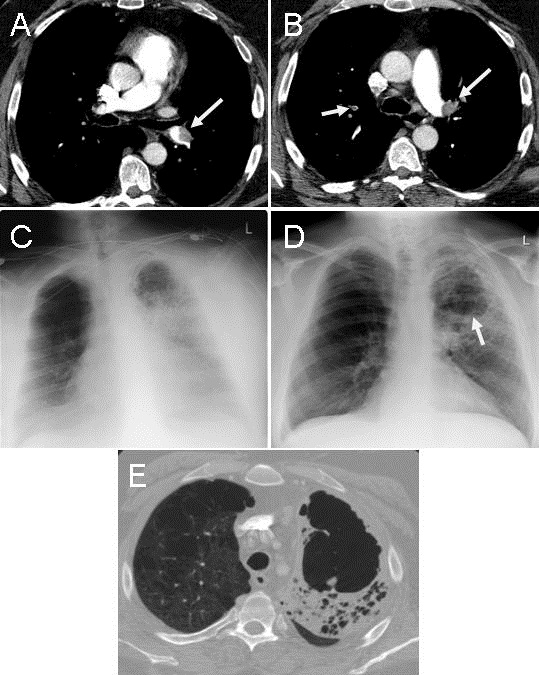
Figure 1. Panels A & B: thoracic CT scan showing multiple pulmonary emboli (arrows). Panel C: frontal chest radiograph showed extensive left lung opacification most dense in the left upper lobe. Panel D: frontal chest radiograph taken 3 weeks later showing mild volume loss of the left upper lobe with a large lucency suggestive of cavitation (arrow). Panel E: thoracic CT scan confirming the cavitation.
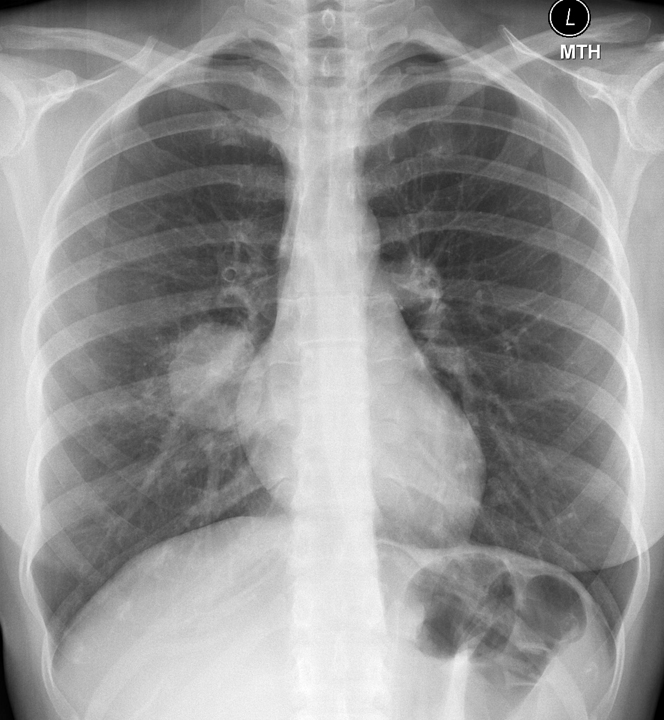
A 49 year old man with a history of COPD presented to the ER with the sudden onset of chest pain at 3:30 AM waking him from sleep. His pain was left sided, felt like broken ribs, and was worse with deep inspiration. He acknowledged some shortness of breath which was worse over baseline for the past couple days without cough or hemoptysis. The patient was tachycardic but comfortable with SpO2 saturation 98% on 2 liters. He had trace edema and pleurisy. Laboratory evaluation was unremarkable except for a WBC count 13,000 X 106 cells/L. Chest x-ray was unremarkable but thoracic CT scan showed pulmonary emboli (PE) involving left upper and lower lobar arteries (Figure 1A and 1B, arrows). Anticoagulation was started and the patient experienced increasing shortness of breath, worsening oxygenation and fever to 102ºF. On Day 2, frontal chest radiograph showed extensive left lung opacification most dense in the left upper lobe (Figure 1C). Hemoglobin dropped from 12 to 9.8 g/dL suggesting alveolar hemorrhage. He improved over the next week but low grade fevers persisted and a chest x-ray taken 3 weeks later showed mild volume loss of the left upper lobe with a large lucency suggestive of cavitation (Figure 1D, Arrow). Thoracic CT confirmed a cavitary lesion in the left apex in the region of prior thrombus with adjacent consolidated atelectasis within a background of emphysema (Figure 1E). The patient was lost to follow up after 6 months of anticoagulation.
Pulmonary infarction is relatively uncommon, occurring in less than 10% of PE, due to dual and collateral blood supply to the lung. Cavitary infarcts are even less common (4% in autopsy studies) and are more likely in those with pulmonary venous hypertension (1). Cavitary infarcts are more likely to occur when the infarct size in larger than 4 cm and most often occurs in the mid and upper lung zones. Despite alveolar hemorrhage, anticoagulation should be continued.
Kenneth S. Knox, MD and Veronica A. Arteaga, MD
Divisions of Pulmonary and Critical Care Medicine and Thoracic Imaging
University of Arizona
Tucson, AZ
Reference
- Libby LS, King TE, LaForce FM, Schwarz MI. Pulmonary cavitation following pulmonary infarction. Medicine (Baltimore). 1985;64(5):342-8. [CrossRef] [PubMed]
Reference as: Knox KS, Arteaga VA. Medical image of the week: PE with infarct and pulmonary cavitation. Southwest J Pulm Crit Care. 2014;9(6):333-4. doi: http://dx.doi.org/10.13175/swjpcc158-14 PDF