SANDSTORM IN THE CHEST?
 Saturday, July 9, 2011 at 7:00AM
Saturday, July 9, 2011 at 7:00AM Manmadha Rao Talluri, M.D.
Department of General Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, INDIA
Reference as: Talluri MR. Sandstorm in the chest? Southwest J Pulm Crit Care 2011;3:1-4. Click here for a PDF version
Corresponding Author:
Dr.Manmadha Rao Talluri
Associate professor
Department of General Medicine
Senior Pulmonologist
Nizams institute of Medical Sciences,
Panjagutta, Hyderabad, India
Phone – 914023489240
Mobile-919490295029
Email: manmadh2277@rediffmail.com
Abstract
A 32 year old female presented with dry cough and progressive breathlessness of one year duration. There was no history suggestive of collagen vascular disease, lung parenchymal infection or allergic airway disease. Clinical evaluation showed basal fine inspiratory crepitations. Radiographic examination of the chest revealed a black pleura line and lung parenchymal calcification. CT scan of the chest demonstrated nodular calcification of lung parenchyma with a “crazy pavement” pattern, which is suggestive of alveolar calcification. Pulmonary function test showed a severe restrictive defect. On transbronchial lung biopsy calcific spherules suggestive of the alveolar microlithiasis were seen. Diagnosis of pulmonary alveolar microlithiasis was made and symptomatic treatment was given, as there is no specific therapy available. The case illustrates an unusual cause of shortness of breath in a young female with striking radiographic features.
Case Summary
History and Physical Examination: A 32 year old woman presented with dry cough and progressive exertional shortness of breath of one year duration. There was no history of bronchial asthma, varicella, rheumatic heart disease, recurrent respiratory tract infections, tuberculosis, occupational dust exposure or connective tissue disease. Furthermore there was no family history of similar complaints but family members were unavailable for screening. Clinical examination showed normal vital signs, facial puffiness with acne and no clubbing. Upper respiratory tract examination was normal. Fine end inspiratory crepitations were heard on lung auscultation. No rhonchi or wheezing was heard. The remainder of the physical examination was normal.
Laboratory Evaluation: Complete blood count, urine examination and renal function tests were within normal limits. Calcium and phosphate were normal. A parathyroid hormone level was not performed. Immunological evaluation showed an antinuclear antibody (ANA) of 1:1 and a rheumatoid factor 42 IU/ml (normal < 30 IU/ml). DsDNA, Anti SS-a, SS-b and U1 RNP were all negative.
Radiography: Radiograph of the chest shown multiple high-density pulmonary nodules in both the lung fields involving all zones with increased density noted in the bases, with a sand storm appearance and a black pleura line (Figure 1).

Figure 1 Radiograph of the chest shows multiple high density pulmonary nodules in both lungs involving all zones with increased density in base as compared to apex, with sand storm appearance and bilateral black pleural lines indicated by the white arrows.
CT scan of the chest is shown in Figure 2.
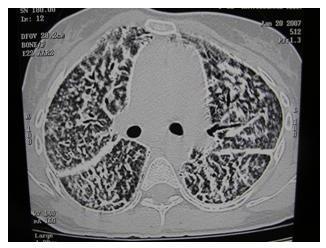
Figure 2. CT scan cross-sectional imaging showing multiple calcific densities in both lungs with thickening and increased density along the fissure and along the mediastinal margin. A black pleural line is noted.
Additional Studies: Pulmonary function test demonstrated a severe restrictive defect. Ultrasound abdomen was normal with no evidence of nephrocalcinosis. Two dimensional echocardiography was normal. Transbronchial biopsy of the lung showed calciphic spherules, which is the hall mark of the pulmonary alveolar microlithiasis (Figure 3).
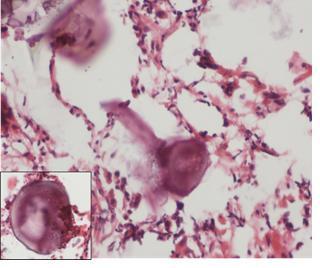
Figure 3. Transbronchial biopsy showing intra-alveolar calcific spherules (H & E, X 200). Insert shows higher magnification of calcific spherules (H&E, X400).
Genetic studies and level of surfactant A and D were not measured.
Clinical Course: The patient was continued on corticosteroids and theophyllines empirically added for dyspnea. Bisphosphonates or chelating agents were not used. She was advised to undergo lung transplantation; which could not be done due to financial constraints. The patient gradually worsened over 2 years and succumbed due to respiratory failure. Permission for an autopsy was not granted.
Discussion
Pulmonary alveolar microlithiasis is a rare disease of unknown etiology, characterized by wide spread laminated clacipherites in alveolar spaces. Other causes of diffuse lung calcification include following tuberculosis, varicella, silicosis, and the metastatic calcification seen with hypercalcemia or renal disease (1).
Pulmonary alveolar microlithiasis is usually sporadic, but an autosomal recessive form has been described in Mediterranean countries (1). The disease is characterized by paucity of symptoms despite wide spread involvement of the lung. Usually presenting in the third or fourth decade of life with cough and dyspnea, pulmonary alveolar microlithiasis usually is a progressive disease with an insidious clinical course resulting in respiratory failure (1,2).
Calcium metabolism has been reported as normal in pulmonary alveolar microlithiasis. Changes in the alveolar membrane secretions resulting in greater alkalinity have been hypothesized to play a major role in the pathogenesis of the disease. The change in alkalinity promotes the intra alveolar precipitation of calcium phosphates. Mutations in the SLC34A2 gene in type II pneumocytes that encodes type IIb sodium phosphate co-transporter have been reported (3). Serum surfactant protein A&D are markedly elevated, which can be useful to monitor the disease activity and progression (4).
Radiograph of the chest is characterized by the presence of a “sand storm” appearance and a black line along the pleura. CT scan usually shows bilateral lung parenchymal nodular calcifications and a “crazy paving” pattern, which is not specific for the diagnosis of pulmonary alveolar microlithiasis (5). Crazy paving has a variety of other causes some of which follow: infectious (Pneumocystis), neoplastic (mucinous bronchoalveolar carcinoma), idiopathic (pulmonary alveolar proteinosis, nonspecific interstitial pneumonitis), inhalational (lipoid pneumonia), and sanguineous disorders (pulmonary hemorrhage syndromes).
Unfortunately, no established treatment is available. Management with corticosteroids, chelating agents, bisphopshonates and bronchoalveolar lavage have all been disappointing. The only viable option for these patients is the bilateral lung transplantation (1).
Conclusion
Pulmonary alveolar microlithiasis is a rare disorder, which should always be considered in the differential diagnosis of calcific micronodular pulmonary lesions.
References
1. Tachibana T, Hagiwara K, Johkoh T. Pulmonary alveolar microlithiasis: review and management. Curr Opin Pulm Med 2009;15:486-490.
2. Castellana G, Gentile M, Castellana R, Fiorente P, Lamorgese V. Pulmonary alveolar microlithiasis: clinical features, evolution of the phenotype, and review of the literature. Am J Med Genet 2002;111:220-224.
3. Huqun, Izumi S, Miyazawa H, Ishii K, Uchiyama B, Ishida T, et al. Mutations in the SLC34A2 gene are associated with pulmonary alveolar microlithiasis. Am. J. Respir. Crit. Care Med 2007;175:263-268.
4. Takahashi H, Chiba H, Shiratori M, Tachibana T, Abe S. Elevated serum surfactant protein A and D in pulmonary alveolar microlithiasis. Respirology 2006;11:330-333.
5. Gasparetto EL, Tazoniero P, Escuissato DL, Marchiori E, Frare E Silva RL, Sakamoto D. Pulmonary alveolar microlithiasis presenting with crazy-paving pattern on high resolution CT. Br J Radiol 2004;77:974-976.
This case was presented at the Great Cases session during the American Thoracic Society meeting in Denver, CO on May 15, 2011. A PowerPoint slide presentation was prepared for than session and a link to the slides is below.

Reader Comments