September 2017 Imaging Case of the Month
 Tuesday, September 5, 2017 at 8:00AM
Tuesday, September 5, 2017 at 8:00AM Michael B. Gotway, MD
Department of Radiology
Mayo Clinic Arizona
Scottsdale, Arizona USA
Clinical History: A 48-year-old woman with no previous medical history presented with complaints of intermittent cough persisting several months following a recent upper respiratory tract infection. No hemoptysis was noted.
Physical examination was largely unremarkable and the patient’s oxygen saturation was 98% on room air. Upon close inspection, the right thorax appeared slightly asymmetrically smaller than the left.
Laboratory evaluation was unremarkable. Quantiferon testing for Mycobacterium tuberculosis was negative, and testing for coccidioidomycosis was unrevealing. Frontal and lateral chest radiography (Figure 1) was performed.
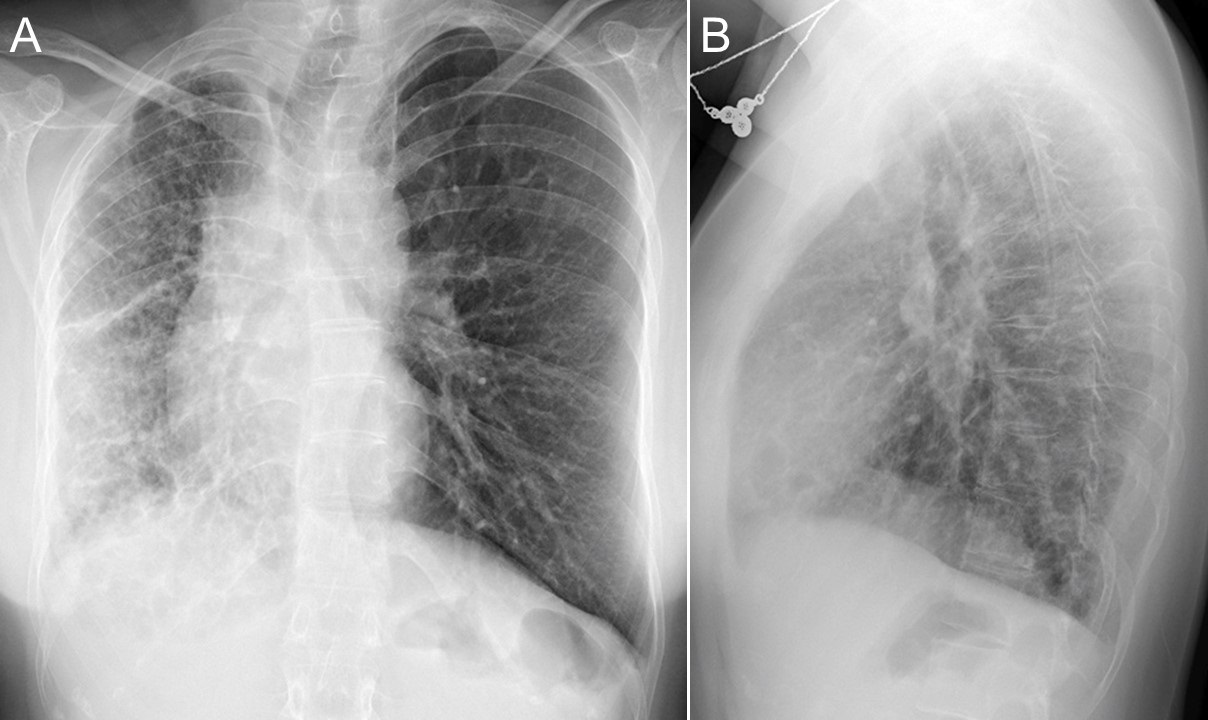
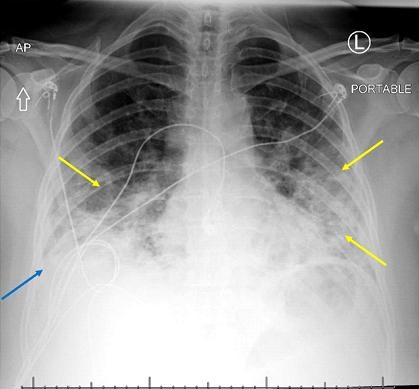
Figure 1. Frontal (A) and lateral (B) chest radiography
Which of the following statements regarding the chest radiograph is most accurate? (Click on the correct answer to proceed to the second of nine pages)
- The chest radiograph shows asymmetric reticulation and interlobular septal thickening
- The chest radiograph shows bilateral reticulation associated with decreased lung volumes
- The chest radiograph shows large lung volumes
- The chest radiograph shows multifocal consolidation and pleural effusion
- The chest radiograph shows small cavitary pulmonary nodules
Cite as: Gotway MB. September 2017 imaging case of the month. Southwest J Pulm Crit Care. 2017;15(3):104-13. doi: https://doi.org/10.13175/swjpcc109-17 PDF