Medical Image of the Week: Pulmonary Infarction- the “Reverse Halo Sign”
 Wednesday, October 18, 2017 at 8:00AM
Wednesday, October 18, 2017 at 8:00AM 
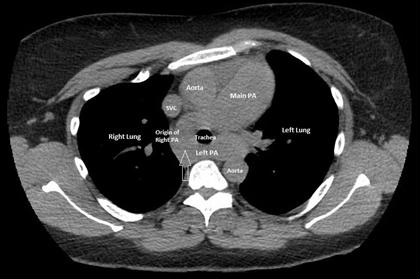
Figure 1. CT Chest with contrast. Two different levels in the same patient displayed on mediastinal windows. Several triangular shaped subpleural lesions with annular peripheral solid appearance are depicted, better characterized in the lung windows below (yellow arrows). Note the partial filling defect (red arrow on B), indicating a non-occlusive thrombus(arrow). Bilateral pleural effusions are also identified.

Figure 2. CT Chest with contrast, lung window corresponding to the levels in Figure 1 above. Note the triangular shaped subpleural lesions with peripheral solid appearance and ground glass center, characteristic of the atoll sign (arrows). As above, bilateral pleural effusions are present.
Pulmonary infarction is a known complication of pulmonary embolism (PE), a common disorder that results in 100,000-200,000 deaths annually in the United States. Computed tomography (CT) is the first-line modality to assess the pulmonary circulation with the ability to directly the visualize pulmonary emboli as well as pleuro-parenchymal abnormalities.
The appearance of a pulmonary infarct varies depending on the degree of ischemic injury in the setting of a dual blood supply to the lung. Infarcts occur more commonly in the periphery of the lung, given, the alternate blood supply by the bronchial arteries, is not as efficient as it is centrally. This location is also favored by the more common occurrence after occlusion of small peripheral arteries of 3 mm or less in caliber.
On CT lung infarcts can take the can take the “reverse halo” sign, also known as the “atoll” sign configuration, representing a focal area of decreased enhancement, and surrounding solid appearance. In the case of lung infarcts, the lesions typically have a broad pleural base triangular form with apex toward the hilum (1). Pathologically this corresponds to a hemorrhagic consolidation. The center of the lesion appears to correspond to aerated non-infarcted lung coexisting side by side with infarcted lung in the same lobule. The broad-based configuration is explained by the fan shaped distribution of the arteries as they extend out into the periphery. The convex border reflects the extravasated blood within the infarcted lung. Once the hemorrhage reabsorbs, the infarct heals completely or may leave behind a linear band of scarring.
From the imaging stand point, the reverse halo sign initially described in cryptogenic organizing pneumonia, has also been noted in patients with fungal disease, granulomatosis with polyangiitis, sarcoidosis and neoplastic disease among others (2).
George R Wu MS IV1, Berndt Schmit MD2, Veronica Arteaga MD2, and Diana Palacio MD2
1Arizona College of Osteopathic Medicine, Midwestern University, Glendale, AZ USA
2Division of Thoracic Imaging, University of Arizona, Tucson, AZ USA
References
- He H, Stein MW, Zalta B, Haramati LB. Pulmonary infarction: spectrum of findings on multidetector helical CT. J Thorac Imaging. 2006;21(1):1-7. [CrossRef] [PubMed]
- Godoy MC, Viswanathan C, Marchiori E, et al. The reversed halo sign: update and differential diagnosis. Br J Radiol. 2012;85(1017):1226-35. [CrossRef] [PubMed]
Cite as: Wu GR, Schmit B, Arteaga V, Palacio D. Medical image of the week: pulmonary infarction- the “reverse halo sign”. Southwest J Pulm Crit Care. 2017;15(4):162-3. doi: https://doi.org/10.13175/swjpcc124-17 PDF