Medical Image of the Week: Mediastinal Lipomatosis
 Wednesday, April 25, 2018 at 8:00AM
Wednesday, April 25, 2018 at 8:00AM 
Figure 1. Chest X-ray showing right sided mediastinal mass.
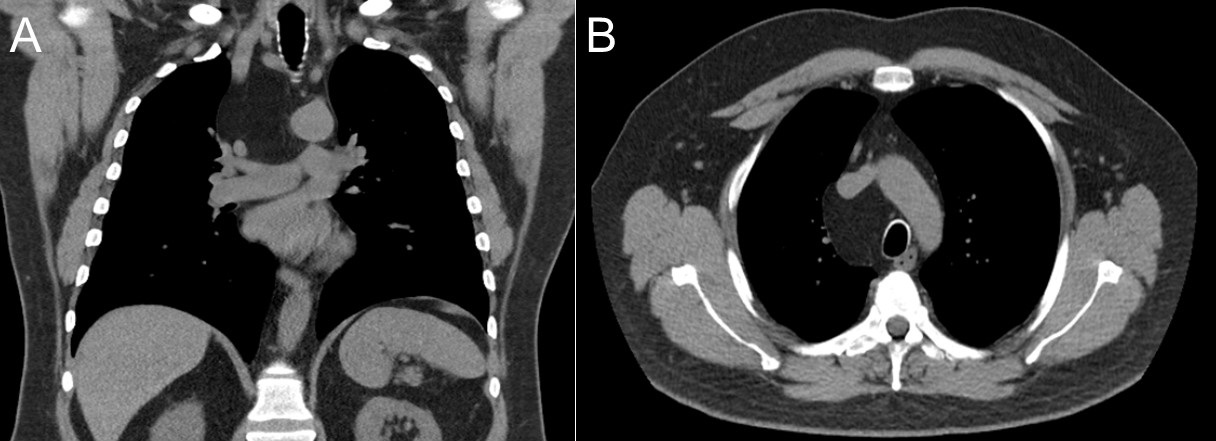
Figure 2. Coronal (A) and axial (B) CT Images showing a right paratracheal homogenously fat-enhancing mass.
A 61-year-old man presented to the pulmonary clinic for evaluation of a chronic cough of 6 months’ duration. Other medical problems included class three obesity, obstructive sleep apnea on CPAP therapy, and hypertension. Chest X-Ray (Figure 1) revealed a right mediastinal mass which then prompted a chest CT to be performed. The chest CT (Figure 2) demonstrated a homogenously enhancing, well circumscribed and fat-attenuating 8 x 5 cm mass in the right paratracheal region without invasion or compression into surrounding structures.
Mediastinal lipomatosis was diagnosed. This is a benign soft tissue tumor made of mature adipocytes that can be seen with obesity, chronic corticosteroid use, and Cushing’s syndrome. They are thought to represent up to 2.3% of all primary mediastinal tumors (1). They are occasionally associated with compression of surrounding structures which can cause superior vena cava syndrome, dry cough, dysphagia, and occasionally arrhythmias (2). Management is typically conservative with weight loss encouraged unless mass effect is present that significantly affects quality of life, in which case surgical options may be explored.
Although this patient’s cough could be due to this lipoma, he also had symptoms of cough possibly exacerbated by severe gastroesophageal reflux disease which was not yet managed. A trial of a proton pump inhibitor was pursued with follow-up arranged to determine if further intervention is necessary.
Bryan Borg MD and James Knepler MD
Department of Medicine
Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine
University of Arizona
Tucson, AZ USA
References
- Gaerte SC, Meyer CA, Winer-Muram HT. Fat-containing lesions of the chest. Radiographics. 2002;22:61-78. [CrossRef] [PubMed]
- Cutilli T, Schietroma M, Marcelli VA, Ascani G, Corbacelli A. Giant cervico-mediastinal lipoma. A clinical case. Minerva Stomatol. 1999 Jan-Feb;48(1-2):23-8. [PubMed]
Cite as: Borg B, Knepler J. Medical image of the week: mediastinal lipomasosis. Southwest J Pulm Crit Care. 2018;16:228-9. doi: https://doi.org/10.13175/swjpcc046-18 PDF


