Medical Image of the Week: Post Pneumonectomy Syndrome
 Wednesday, June 6, 2018 at 8:00AM
Wednesday, June 6, 2018 at 8:00AM 
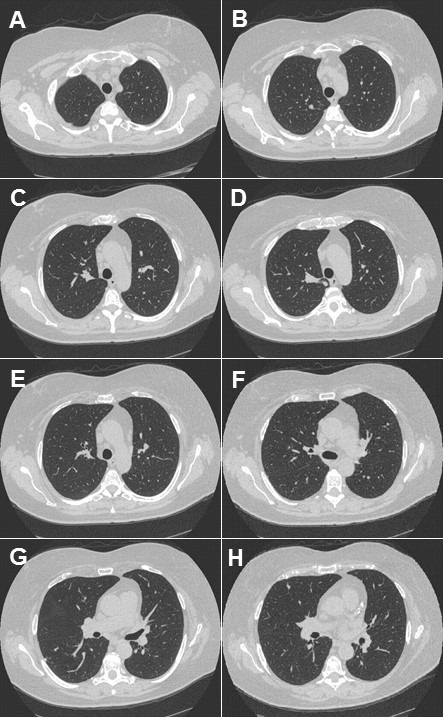
Figure 1.Computed tomography of the chest. Panel A: lung windows reveal hyperexpansion of right lung with extreme shift of mediastinum to the left hemithorax. Panel B: mediastinal windows reveals rotation of the heart toward midline.
A 73 year-old woman with a history of left pneumonectomy in 2012 for Stage IB adenocarcinoma of the lung presented to the outpatient pulmonary clinic with dyspnea on exertion and fatigue. Computed tomography of the chest reveals hyperexpansion of the right lung with complete shift of the heart and mediastinal structures into the left hemithorax, (Figure 1). There is tethering of the right mainstem bronchus and right-sided vessels with a stretched configuration of the trachea, esophagus and right-sided vasculature. The heart is rotated toward the midline. The central airways are patent, however, the tethering and rotation of the mediastinal structures are concerning for post-pneumonectomy syndrome (PPS).
PPS is a rare and late complication after pneumonectomy and results from extreme shift and rotation of the mediastinum. Symptoms can include progressive dyspnea, cough, inspiratory stridor and recurrent pneumonia (1). Dyspnea can be caused by bronchial compression or by compression of the pulmonary vein (2). Dysphagia and acid reflux can result from esophageal compression (3). PPS is more common after right pneumonectomy, however cases following left pneumonectomy are well described. Treatment options include surgical correction using saline‐filled tissue expanders to restore normal mediastinal position (4).
Billie Bixby MD and James Knepler MD
Division of Pulmonary, Allergy, Critical Care and Sleep
University of Arizona
University Medical Center Tucson
Tucson, AZ USA
References
- Valii, AM, Maziak DE, Shamii FM, Matzinger RF. Postpneumonectomy syndrome: recognition and management. Chest. 1998; 114:1766. [CrossRef] [PubMed]
- Partington SL, Graham A, Weeks SG. Pulmonary vein stenosis following left pneumonectomy: a variant contributor to postpneumonectomy syndrome. Chest. 2010;137(1):205-6. [CrossRef] [PubMed]
- Soll C, Hahnloser D, Frauenfelder T, Russi EW, Weder W, Kestenholz PB. The postpneumonectomy syndrome: Clinical presentation and treatment. Eur J Cardiothorac Surg. 2009; 35: 319-24. [CrossRef] [PubMed]
- Jung JJ, Cho JH, Kim HK, et al. Management of post‐pneumonectomy syndrome using tissue expanders. Thoracic Cancer. 2016;7(1):88-93. [CrossRef] [PubMed]
Cite as: Bixby B, Knepler J. Medical image of the week: post pneumonectomy syndrome. Southwest J Pulm Crit Care. 2018;16(6):332-3. doi: https://doi.org/10.13175/swjpcc071-18 PDF