November 2019 Imaging Case of the Month: A 56-Year-Old Woman with a Rash
 Friday, November 1, 2019 at 8:00AM
Friday, November 1, 2019 at 8:00AM Michael B. Gotway, MD
Department of Radiology
Mayo Clinic Arizona
Scottsdale, AZ USA
Clinical History: A 56-year-old post-menopausal woman with a remote history of asthma and asymptomatic uterine fibroids presented with a macular-papular rash over the upper chest, upper medial left forearm, and medial legs, without scaling that has intermittently recurred over the previous few years. The rash is unaccompanied by fever, chills, rigors, abdominal pain, cough, conjunctivitis, urethritis, or any other mucocutaneous lesions. The patient did not note any seasonal relationships or association with food, and the rash regresses promptly with H1 or H2-blocker therapy.
The patient’s past medical history was otherwise unremarkable. Her surgical history was positive only for a laparoscopic left inguinal hernia repair 7 years earlier. The patient indicated she was neither a smoker nor a drinker. Her medications included an as-needed albuterol inhaler, a steroid inhaler, a nasal steroid spray, a multivitamin, and a topical steroid.
The patient’s physical examination showed normal vital signs, although her pulse rate was 95 beats / minute. The physical examination was otherwise entirely within normal limits aside from her presenting complaint of rash; in particular, her lungs were clear to auscultation.
About 2 weeks later, the patient began to complain of myalgias and some wheezing in addition to her rash, with some mild fatigue as well. She denied other complaints, such as coryza, cough, nasal drainage, ear pain, and neck pain or stiffness. At repeat physical examination, her lungs remained clear to auscultation; no wheezing was noted. A dermatology consult suggested that the rash was most consistent with atopic dermatitis, for which a topical steroid was prescribed.
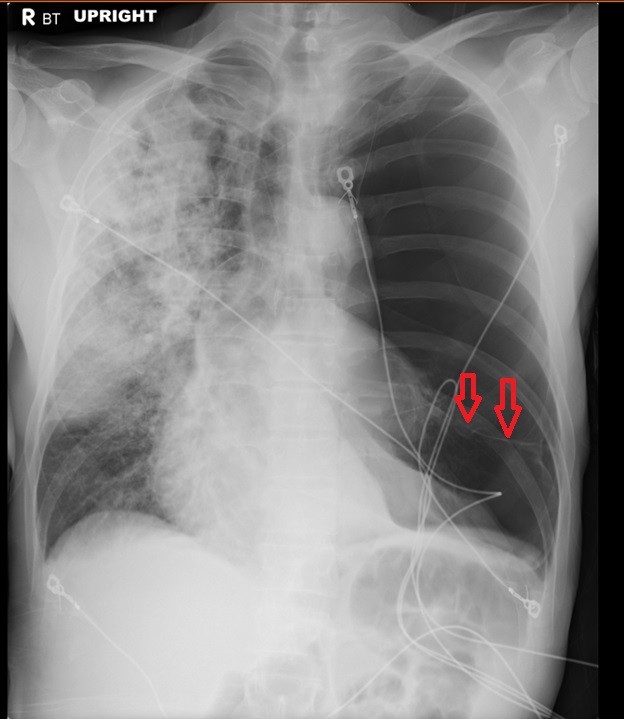
Basic laboratory data showed a white blood cell count in the normal range, mild anemia (hemoglobin / hematocrit = 11.5 mg/dL / 34.7%), a normal platelet count, normal serum chemistries and renal function parameters, and normal liver function tests aside from a mildly elevated alkaline phosphatase level of 145 U/L147 (normal, 35 – 104 U/L). A C-reactive protein level was elevated at 38.5 mg/L (normal, ≤8 mg/L). The patient was referred for chest radiography (Figure 1).

Figure 1. Frontal chest radiograph.
Which of the following statements regarding the chest radiograph is most accurate? (Click on the correct answer to be directed to the second of twelve pages)
- The chest radiograph shows mediastinal and peribronchial lymph node enlargement
- The chest radiograph shows bilateral consolidation
- The chest radiograph shows cavitary lung disease
- The chest radiograph shows findings suggesting increased pressure pulmonary edema
- The chest radiograph shows numerous small nodules
Cite as: Gotway MB. November 2019 imaging case of the month: a 56-year-old woman with a rash. Southwest J Pulm Crit Care. 2019;19(5):127-43. doi: https://doi.org/10.13175/swjpcc065-19 PDF