Medical Image of the Week: Right Main Bronchus Obstruction in a Young Man
 Wednesday, August 14, 2013 at 8:04AM
Wednesday, August 14, 2013 at 8:04AM 
Figure 1. Panel A: chest x-ray at presentation. Panel B: CT scan at presentation.
Figure 2. Panel A: Mass encroaching the carina. Panel B: Near total occlusion of the right main bronchus.
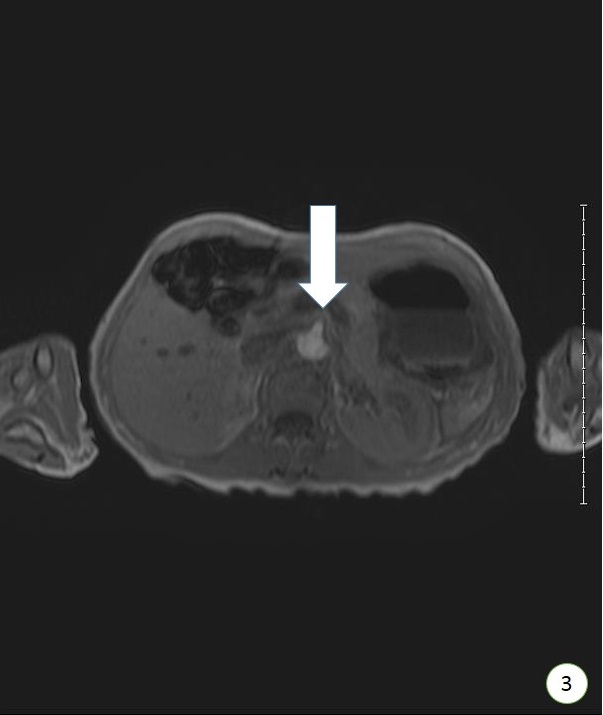
Figure 3. Tissue removed during bronchoscopy.
Figure 4. Post-procedure image.
The patient is a 22 year old man with long standing history of recurrent laryngeal papillomatosis since childhood.
He was referred to the hospital by his ENT surgeon and pulmonology was consulted for evaluation of pneumonia and lung mass. Initial chest x-ray (Figure 1A) demonstrated a white out of the right lung. A CT scan (Figure 1B) obtained showed a pedunculated mass in the right main stem and extensive post obstructive pneumonia. At bronchoscopy, a near total occlusion of the right main stem bronchus was seen with extension in to the trachea (Figure 2). Piecemeal excision of the mass was done using multiple snare passes (Figure 3). The right main stem was subsequently cleared and the distal airway found patent with no endobronchial lesions (Figure 4). The mass continued to obstruct the right upper lobe take off completely.
Pathology was consistent with squamous papilloma with dysplasia. Further work up revealed no metastatic disease and the patient is undergoing evaluation for treatment strategies.
Laryngeal papillomatosis is a human papilloma virus (HPV) associated disease that may progress to malignancy, not only of the larynx but anywhere in the aero-digestive tract.
Bhupinder Natt MD, Nauman Hamid MD, and James Knepler MD
Division of Pulmonary, Allergy, Critical Care and Sleep Medicine.
University of Arizona
Tucson, Arizona.
Reference as: Natt B, Hamid N, Knepler J. Medical image of the week: right main bronchus obstruction in a young man. Southwest J Pulm Crit Care. 2013;7(2):100-2. doi: http://dx.doi.org/10.13175/swjpcc107-13 PDF