Medical Image of the Week: Oligemic Lung Field
 Wednesday, January 15, 2014 at 8:00AM
Wednesday, January 15, 2014 at 8:00AM A Sinister Sign of Acute Pulmonary Embolism?
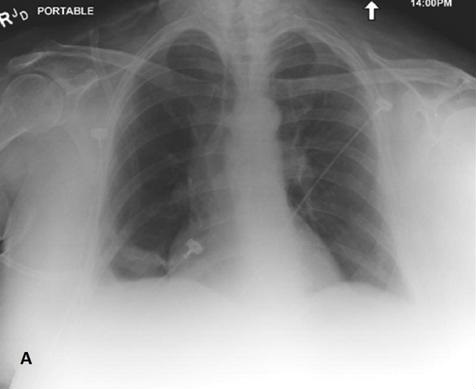
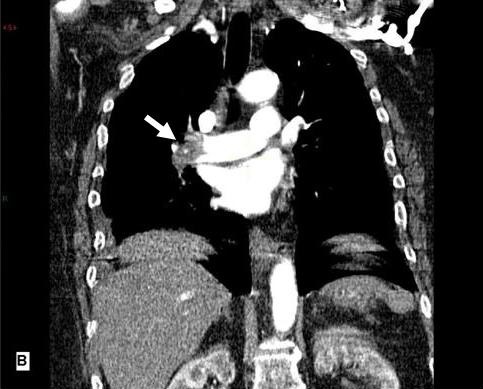
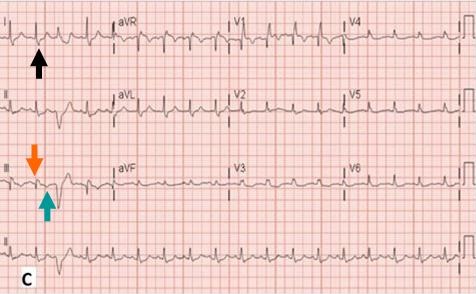
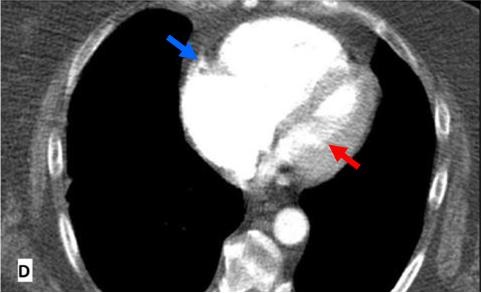
Figure 1. Panel A: The chest x-ray showed decreased vascular markings in the right lung field (oligemic right lung field) and reduced prominence of right pulmonary artery. There is also a small opacity in right lower lung field possibly a pulmonary infarct. Panel B: A Coronal section of the computed tomographic pulmonary angiography showing a large thrombus in the right pulmonary artery (white arrow). Panel C: A 12-lead EKG shows sinus tachycardia, right bundle branch block, deep S wave in lead I (black arrow), deep q wave (orange arrow) and inverted T-wave (green arrow) in lead III. Panel D: A computed tomographic pulmonary angiography showing an enlarged right ventricle (blue arrow) compressing the left ventricle (red arrow).
A 67 year-old woman presented with pleuritic, non-radiating chest pain of sudden onset. She was anxious, diaphoretic, and tachycardic.
The chest radiograph (Figure 1A) showed decreased vascular markings in the entire right lung field (oligemic right lung field) and reduced prominence of the right pulmonary artery. A small opacity in right lower lung field was suspicious for a pulmonary infarct. A follow-up computed tomographic pulmonary angiography (CTA) showed a large embolus in right pulmonary artery and a smaller embolus in the subsegmental left pulmonary artery (Figure 1B). Twelve-lead electrocardiogram (EKG) findings were notable for a new onset right bundle branch pattern, deep S wave in lead I, with a q-wave and inverted T-wave in Lead III (Figure 1C). A 2-Dimentional echocardiogram showed a massively dilated and hypokinetic right ventricle. The CTA also revealed that the massively distended right ventricle with a deviated interventricular septum was compressing the left ventricle (Figure 1D). Venous duplex study of lower extremities showed an acute thrombosis of the right popliteal vein.
The patient showed marked clinical improvement after the infusion of tissue plasminogen activator (tPA) and heparin. A chest x-ray obtained 2 days later showed resolution of right sided oligemia. On Day 6, the right bundle branch block had resolved.
Radiographic findings in acute pulmonary embolism (PE) are uncommon. The Westermark sign (oligemia), Hampton hump and prominent central pulmonary artery are infrequently seen in acute PE. Westermark sign of an entire side lung field is rare, sinister sign of a large burden pulmonary embolism. If identified early, this sign can be invaluable in early recognition and management.
Suman B. Thapamagar MBBS, Ramya Mallareddy MD, Ilya Lantsberg MD
Easton Hospital, Drexel University, Department of Internal Medicine, 250 S. 21st Street, Easton, PA 18042
Reference
- Agnelli G, Becattini C. Acute pulmonary embolism. N Engl J Med. 2010;363(3):266-74. [CrossRef] [PubMed]
Reference as: Thapamagar SB, Mallareddy R, Lantsberg I. Medical image of the week: oligemic lung field. Southwest J Pulm Crit Care. 2014:8(1):48-9. doi: http://dx.doi.org/10.13175/swjpcc163-13 PDF



