Medical Image of the Week: Diffuse Axonal Injury
 Wednesday, December 9, 2015 at 8:00AM
Wednesday, December 9, 2015 at 8:00AM 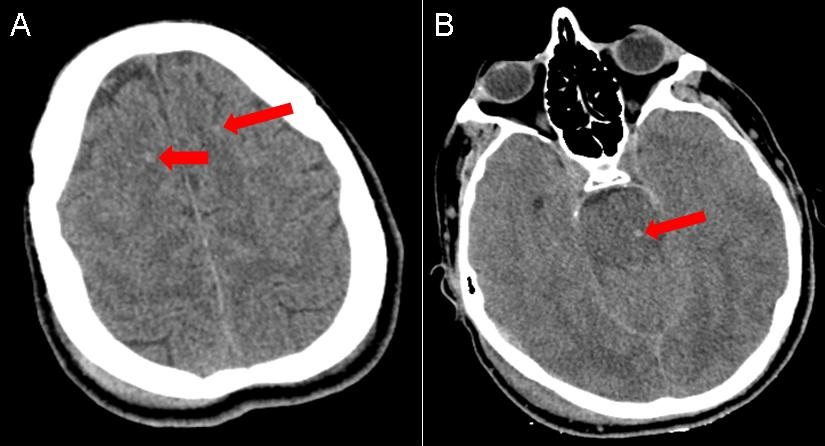
Figure 1. Panel A: Non-contrast CT of the head demonstrating hyperdense foci at the gray-white junction of the cortex and subcortical white matter (red arrows). Panel B: Hyperdense focus in the pons (red arrow).
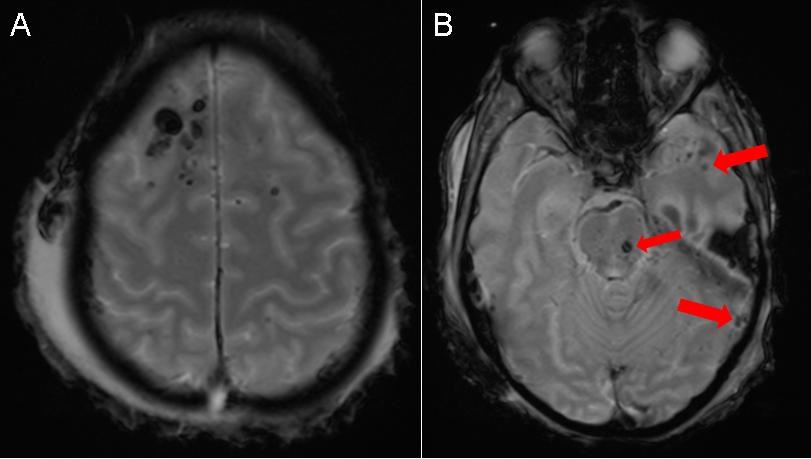
Figure 2. MRI of the brain with a gradient recall echo (GRE) sequence demonstrating more pronounced hypointense foci consistent with hemorrhage.
An 18-year-old man without any significant past medical history presented to the emergency room trauma bay as an unrestrained passenger involved in a head-on collision at 85 mph. In the emergency room, he was found to have a GCS of 6 and was intubated for airway protection. A non-contrast CT of the head demonstrated hyperdense foci in the frontal lobes at the gray-white junction (Figure 1A) and a hyperdense focus in the pons (Figure 1B) consistent with punctate hemorrhages. An MRI of the brain with a gradient recall echo (GRE) sequence (Figure 2) demonstrated more pronounced hypointense foci consisent with hemorrhage. In the setting of the patient’s deceleration injury, the summation of his clinical and imaging findings was consistent with diffuse axonal injury.
Diffuse axonal injury (DAI) is pattern of closed head injury that results in a traumatic shear injury to the neuronal axons secondary to sudden deceleration and change in angular momentum. This pattern of injury often occurs at the interface between tissues of differing density such as the gray-white junction of the cerebral cortex and subcortical white matter. DAI can also be seen in deeper portions of the brain, such as the corpus callosum and brainstem, that are relatively fixed compared with more superficial portions of the brain resulting in greater rotational/ shear stress forces focused in these locations during sudden deceleration. Visible lesions on CT often underestimate the extent of neuronal injury (often described as the “tip of iceberg”), and neuronal injury is better delineated on MRI.
Most patients present with an immediate coma necessitating intubation for airway protection. In mild cases, patients often experience mild traumatic brain injury characterized by heachaces, mild cognitive impairment, and personality changes. In more severe cases, DAI can result in a persistent vegetative state. Treatment is supportive in all cases.
Jack Hannallah, MD1; Tammer Elaini, MD2; Kelly Wickstrom, DO3; Rorak Hooten, MD3; Michael Habib, MD2
Departments of 1Surgery,2Pulmonary/Critical Care, and 3Internal Medicine
University of Arizona
Tucson, AZ USA
References
- Yanagawa Y, Sakamoto T, Takasu A, Okada Y. Relationship between maximum intracranial pressure and traumatic lesions detected by T2*-weighted imaging in diffuse axonal injury. J Trauma. 2009;66(1):162-5. [CrossRef] [PubMed]
- Tong KA, Ashwal S, Holshouser BA, Shutter LA, Herigault G, Haacke EM, Kido DK. Hemorrhagic shearing lesions in children and adolescents with posttraumatic diffuse axonal injury: improved detection and initial results. Radiology. 2003;227(2):332-9. [CrossRef] [PubMed]
Cite as: Hannallah J, Elaini T, Wickstrom K, Hooten R, Habib M. Medical image of the week: diffuse axonal injury. Southwest J Pulm Crit Care. 2015;11(6):264-5. doi: http://dx.doi.org/10.13175/swjpcc121-15 PDF


