July 2017 Imaging Case of the Month
 Thursday, July 6, 2017 at 8:00AM
Thursday, July 6, 2017 at 8:00AM Michael B. Gotway, MD
Department of Radiology
Mayo Clinic Arizona
Scottsdale, Arizona USA
Clinical History: A 56-year-old man with no significant past medical history presented with complaints of cough, shortness of breath, and productive sputum. Frontal and lateral chest radiography (Figure 1) was performed.
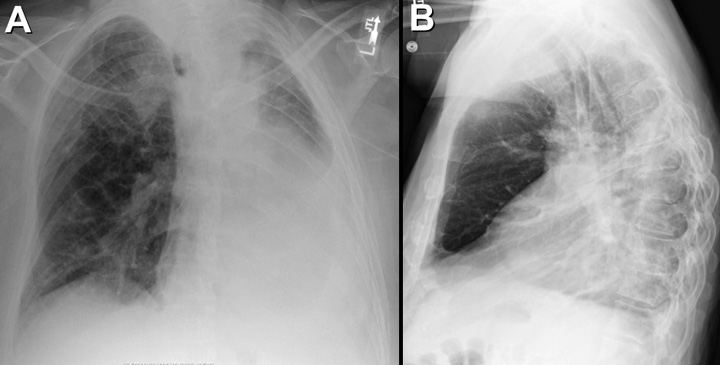
Figure 1. Frontal (A) and lateral (B) chest radiography.
Which of the following statements regarding the chest radiograph is most accurate? (Click on the corect answer to proceed to the second of nine pages)
- The chest radiograph shows a diffuse linear, interstitial pattern
- The chest radiograph shows a large pleural effusion
- The chest radiograph shows a mediastinal mass
- The chest radiograph shows numerous small nodules
- The chest radiograph shows right lower lobe consolidation
Cite as: Gotway MB. July 2017 imaging case of the month. Southwest J Pulm Crit Care. 2017;15(1):17-27. doi: https://doi.org/10.13175/swjpcc090-17 PDF



