Medical Image of the Week: Valley Fever Cavity with Fungus Ball
 Wednesday, May 16, 2018 at 8:00AM
Wednesday, May 16, 2018 at 8:00AM 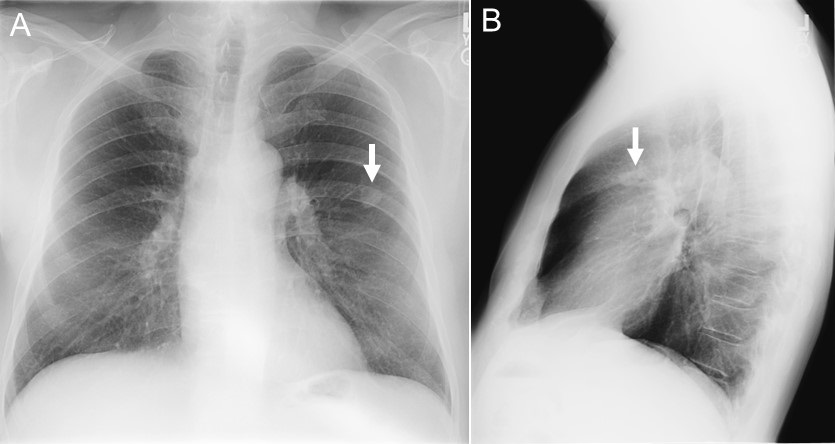
Figure 1. Chest x-ray taken in 2004 showing pulmonary nodule (arrows).
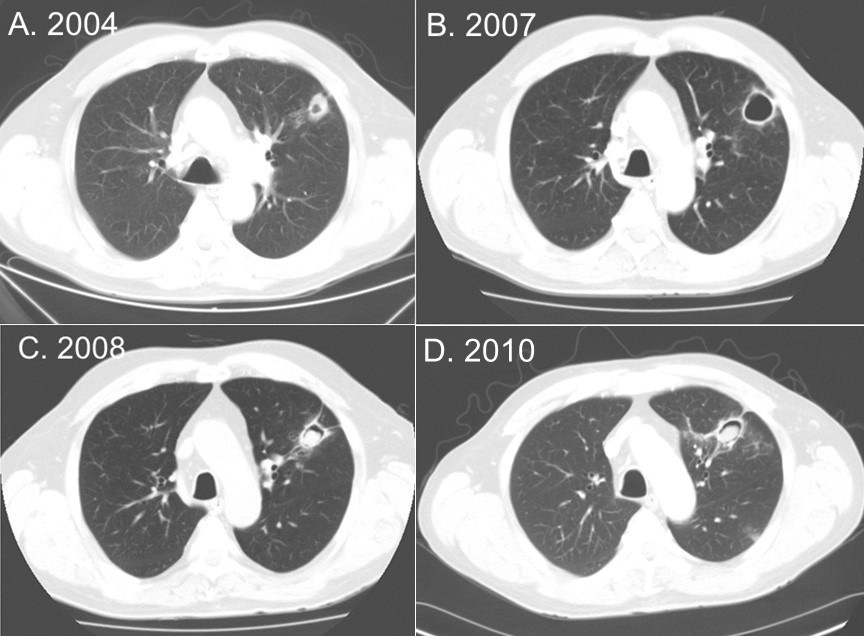
Figure 2. A: Thoracic CT scan in lung windows from 2004 showing the pulmonary nodule with cavitation. B: CT scan from 2007 showing thin-walled cavity. C: CT scan from 2008 showing fungus ball inside the cavity. D: CT scan from 2010 showing the continued presence of the fungus ball inside the cavity.
A 72-year-old man was seen in 2010 because of hemoptysis. In 2004 a routine chest x-ray discovered a new pulmonary nodule (Figure 1, Figure 2A). Coccioidomycosis by complement fixation and IgM were negative but IgG was elevated at 0.203 (upper limit of normal 0.150). A transthoracic needle biopsy revealed a granuloma without malignancy and no growth of any organisms. He was followed because he was asymptomatic. He remained asymptomatic but developed a thin-walled cavity (Figure 2B). However, beginning in 2008 he developed a cough with occasional hemoptysis. His thoracic CT scan was repeated and was interpreted as showing findings consistent with a fungus ball (Figure 2C). He was treated with fluconazole for about 6 months but his hemoptysis persisted and therapy was switched to itraconazole. His hemoptysis persisted although it was somewhat improved. A repeat CT scan performed in 2010 (Figure 2D) continued to show the fungus ball. He was referred to pulmonary and bronchoscopy revealed no other source of the hemoptysis; stains and cultures were negative; and he was referred to thoracic surgery for resection.
Hemoptysis from coccioidomycosis is unusual and should prompt a search for other causes (1). These could include bronchitis, malignancy, or rarely, a fungus ball as in our case. When hemoptysis is present with a fungus ball, treatment with fluconazole, itraconazole or amphotericin B is often advised although descriptions are limited to case reports. When hemoptysis persists despite drug therapy, resection of the cavity has been performed (2).
Richard A. Robbins, MD
Phoenix Pulmonary and Critical Care Research and Education Foundation
Gilbert, AZ USA
Reference
- Galgiani JN, Knox K, Rundbaken C, Siever J. Common mistakes in managing pulmonary coccidioidomycosis. Southwest J Pulm Crit Care. 2015;10(5):238-49. [CrossRef]
- Thadepalli H, Salem FA, Mandal AK, Rambhatla K, Einstein HE.Pulmonary mycetoma due to Coccidioides immitis. Chest. 1977 Mar;71(3):429-30. [PubMed]
Cite as: Robbins RA. Medical image of the week: valley fever cavity with fungus ball. Southwest J Pulm Crit Care. 2018;16(5):281-2. doi: https://doi.org/10.13175/swjpcc064-18 PDF

