Medical Image of the Month: Hot Tub Lung
 Sunday, September 2, 2018 at 8:00AM
Sunday, September 2, 2018 at 8:00AM 
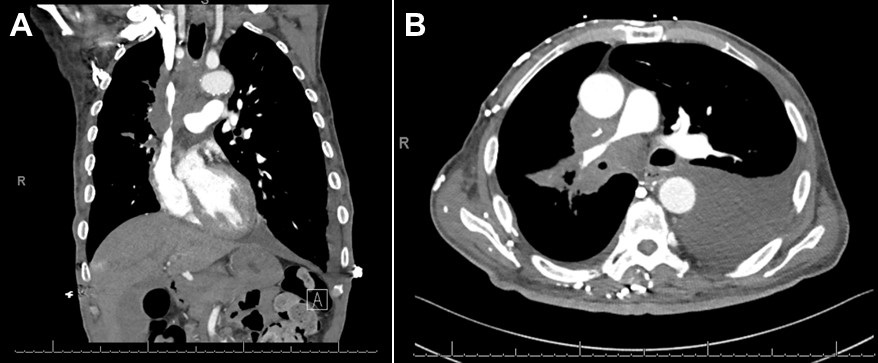
Figure 1. Chest radiograph showing diffuse micronodular disease.
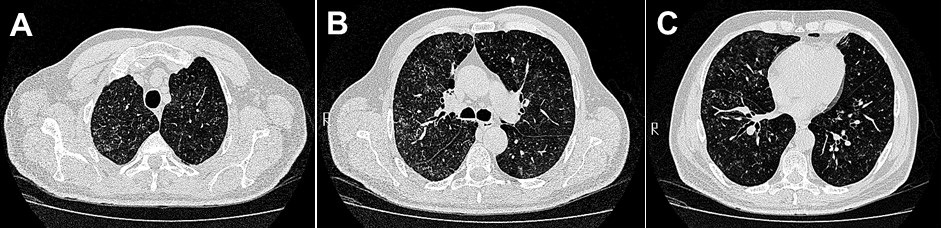
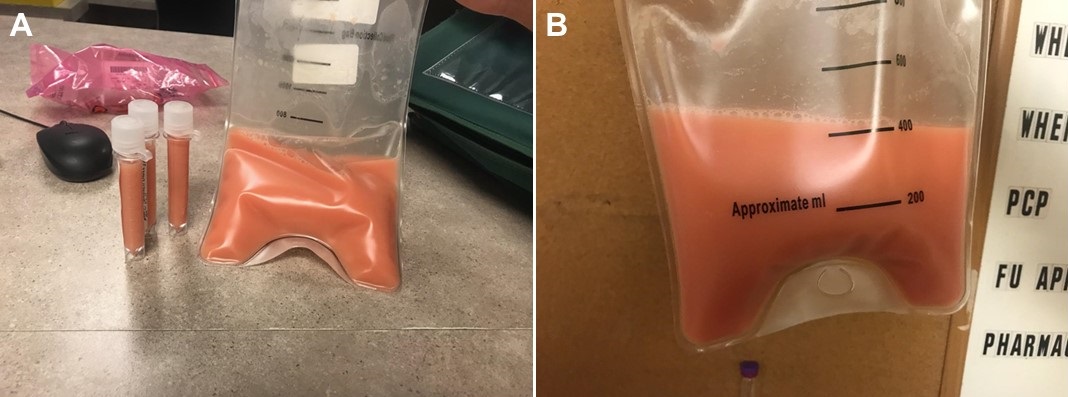
Figure 2. Representative images from the thoracic CT scan confirming diffuse micronodular disease with a centrilobular distribution.
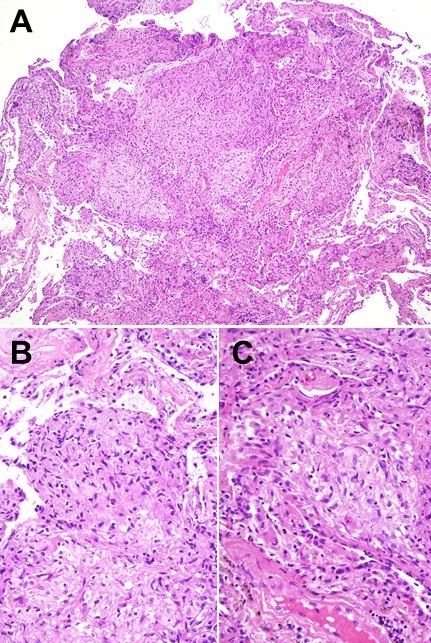
Figure 3. Lung biopsy from VATS showing granulomas. Panel A: Low power view. Panels B & C: High power views.
The patient is a 65-year-old man with progressively worsening shortness of breath for 2 months. He had a past medical history of type 2 diabetes mellitus, hypertension, hypothyroidism and a 40 pack-year history of smoking. He suffered from chronic neck pain and sought relief by spending up to 6 hours daily in a hot tub. Chest x-ray (Figure 1) showed numerous small nodules which were confirmed on thoracic CT (Figure 2). The nodules spared the pleural space consistent with a centrilobular distribution. Bronchoscopy with bronchoalveolar lavage grew Mycobacterium avium intracellulare (MAC) and a lung biopsy obtained by video-assisted thorascopic surgery (VATS) showed non-caseating granulomas (Figure 3). Culture of the hot tub water also grew MAC. He was advised to stop using the hot tub and was treated with prednisone, clarithromycin, rifampin and ethambutol. He rapidly improved though he stopped his therapy after about 3 weeks due to intolerance. He continued to do well and was asymptomatic when last seen.
Hot tub lung may represent either an infectious process or a hypersensitivity pneumonitis to MAC inhaled from the hot tub. Improvement is usually seen with prednisone, anti-MAC therapy or both (1). The thoracic CT findings are consistent with subacute hypersensitivity pneumonitis including areas of ground-glass attenuation, centrilobular nodules, and air trapping on expiratory images (2). Granulomas, a compact collection of macrophages, are a nonspecific finding seen in both infectious (mycobacteria and fungi) and noninfectious lung diseases (sarcoidosis, hypersensitivity pneumonitis, hot tub lung, and several others) (3). In our patient’s case the clinical history, radiologic findings, lung histology and rapid improvement with removal of MAC exposure are all consistent with hot tub lung.
Allen R. Thomas, MD
Phoenix VA
Phoenix, AZ USA
References
- Khoor A, Leslie KO, Tazelaar HD, Helmers RA, Colby TV. Diffuse pulmonary disease caused by nontuberculous mycobacteria in immunocompetent people (hot tub lung). Am J Clin Pathol. 2001 May;115(5):755-62. [CrossRef] [PubMed]
- Hartman TE, Jensen E, Tazelaar HD, Hanak V, Ryu JH.CT findings of granulomatous pneumonitis secondary to Mycobacterium avium-intracellulare inhalation: "hot tub lung". AJR Am J Roentgenol. 2007 Apr;188(4):1050-3. [CrossRef] [PubMed]
- Hutton Klein JR, Tazelaar HD, Leslie KO, Colby TV. One hundred consecutive granulomas in a pulmonary pathology consultation practice. Am J Surg Pathol. 2010 Oct;34(10):1456-64. [CrossRef] [PubMed]
Cite as: Thomas AR. Medical image of the month: hot tub lung. Southwest J Pulm Crit Care. 2018;17(3):93-4. doi: https://doi.org/10.13175/swjpcc077-18 PDF