March 2014 Imaging Case of the Month
 Monday, March 3, 2014 at 8:00AM
Monday, March 3, 2014 at 8:00AM Michael B. Gotway, MD
Department of Radiology
Mayo Clinic Arizona
Scottsdale, AZ
Clinical History: A 60-year-old man with a history of severe asthmatic bronchitis presented with a 6 week history of intermittent fever, productive cough, shortness of breath, and decreased appetite. Four weeks earlier the patient was presumptively treated with amoxicillin for presumed community-acquired pneumonia, with some improvement, but his symptoms recurred 10 days following completion of his course of therapy. The patient also thought he was diagnosed with a COPD exacerbation during this time period and was treated with a short course of corticosteroids without improvement.
The patient was seen by his pulmonologist who noted decreased breath sounds over the right thorax, and referred the patient to the emergency room.
In the emergency room, a leukocytosis (white blood cell count = 17.4 x 109 / L with neutrophilia) was noted. Broad-spectrum antibiotic coverage was re-instituted and frontal chest radiography (Figure 1) was performed.
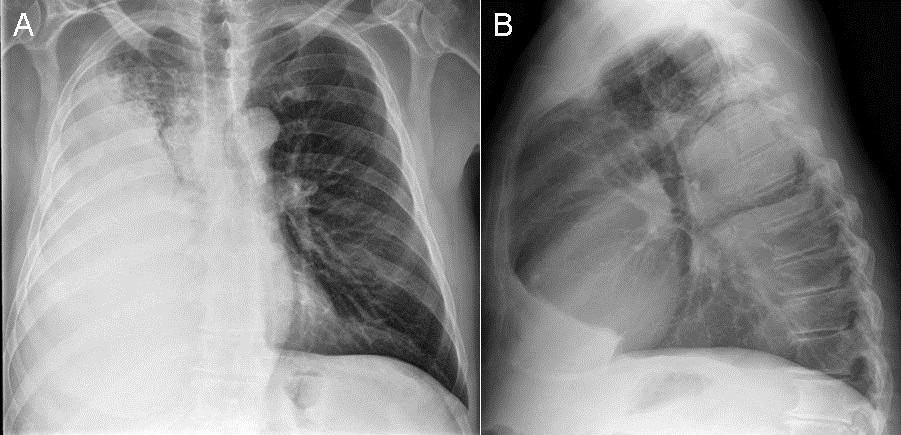
Figure 1: Frontal (A) and lateral (B) chest radiography
Which of the following statements regarding the chest radiograph is most accurate? (Click on the correct answer to move to the next panel)
- The chest radiograph homogeneous complete right lung consolidation
- The chest radiograph shows a right-sided mediastinal mass
- The chest radiograph shows homogeneous right lung opacity suggesting right lung collapse
- The chest radiograph shows homogeneous right lung opacity suggesting a large right pleural effusion
- The chest radiograph shows multiple nodules
Reference as: Gotway MB. March 2014 imaging case of the month. Southwest J Pulm Crit Care. 2014:8(3):161-9. doi: http://dx.doi.org/10.13175/swjpcc015-14 PDF