Medical Image of the Week: Acute Aortic Dissection
 Wednesday, April 16, 2014 at 8:00AM
Wednesday, April 16, 2014 at 8:00AM 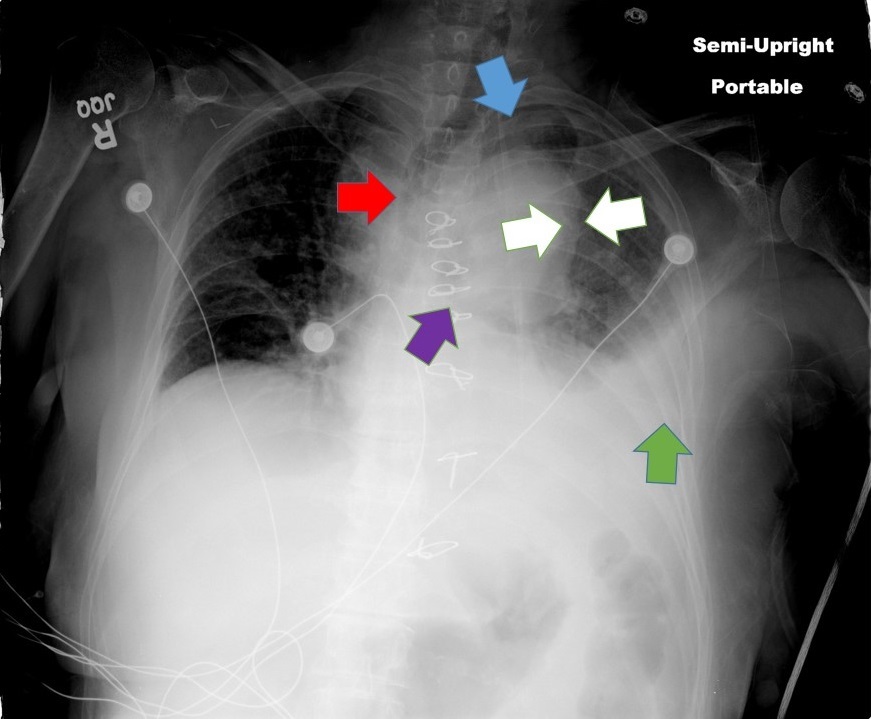
Figure 1. Acute aortic dissection presenting with the following radiographic signs: rightward deviation of the trachea (red arrow); left apical pleural capping (blue arrow); aortic “double-calcium” sign (between white arrows); depression of the left bronchus (purple arrow); pleural effusion (green arrow); widened mediastinum and loss of the aorto-pulmonary window (not labeled).
The patient was a 75 year old woman with a past medical history of uncontrolled hypertension and recent type-A aortic dissection post graft repair. She presented with a sudden onset of sharp mid-back pain which awoke her from sleep. In the emergency room a chest x-ray revealed numerous features consistent with a de novo type B aortic dissection which was ultimately confirmed by magnetic resonance angiography of the chest and abdomen. This dissection extended from the left subclavian artery to the right renal artery. There was no evidence of end-organ mal-perfusion and the patient was medically managed by way of blood pressure control.
Seth Assar, MD; Thien Vo, MD; Jarrod Mosier, MD
The University of Arizona College of Medicine, Tucson, Arizona
Reference
Bansal V, Lee J, Coimbra R. Current diagnosis and management of blunt traumatic rupture of the thoracic aorta. J Vasc Bras. 2007;6(1):64-7. [CrossRef]
Reference as: Assar S, Vo T, Mosier J. Medical image of the week: acute aortic dissection. Southwest J Pulm Crit Care. 2014;8(4):234. doi: http://dx.doi.org/10.13175/swjpcc039-14 PDF

