Medical Image of the Week: Idiopathic Pulmonary Artery Hypertension
 Wednesday, August 6, 2014 at 8:00AM
Wednesday, August 6, 2014 at 8:00AM 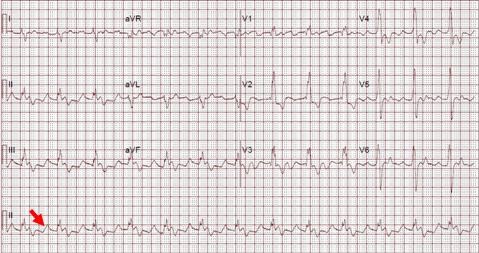
Figure 1. EKG showing sinus rhythm, right bundle branch block and peaked ('pulmonary') p waves (arrow).

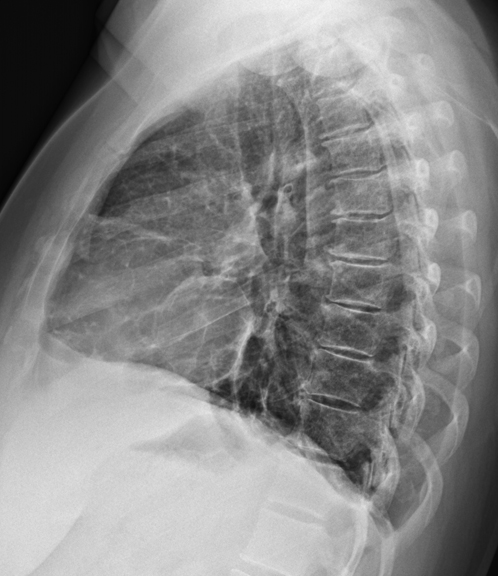
Figure 2. Two view chest X-ray showing right ventricular hypertrophy (arrows, note filling of the retrosternal space by an enlarged right ventricle in the lateral view) and enlarged central pulmonary arteries (arrowhead).

Figure 3. Axial CT angiogram of the chest below the carina showing dilated pulmonary artery (diameter of pulmonary artery greater than aorta, arrow).


Figure 4. Panel A: Parasternal short axis view shows septal bowing to the left, a severely dilated right ventricle and a D-shaped left ventricle. Panel B: Four chamber view shows right atrial and ventricular dilatation.
A 39-year-old woman presented to the clinic with a history of progressive shortness of breath of 6-month duration associated with bilateral lower extremity edema, fatigue, lightheadedness, palpitations and occasional substernal chest pain. Her past medical history was unremarkable other than mild anemia. On physical exam her respiratory rate was 20 breaths per minute and O2 saturation 94% on room air by pulse oximetry. There was jugular venous distention at 12 cm, 2+ bilateral lower extremity edema, a 5/6 systolic murmur over the left sternal border with a sternal heave. Labwork was unremarkable except for an elevated BNP 657 (normal value < 100 pg/mL).
EKG (Figure 1) showed sinus rhythm with right bundle branch block. A 2-view chest X-ray (Figure 2) showed an enlarged right ventricle as well as dilated pulmonary arteries with no parenchymal infiltrates. CT angiography confirmed CXR findings (Figure 3) and was negative for pulmonary embolism. A 2D echocardiogram revealed a preserved left ventricle ejection fraction with right ventricular pressure of 80 mmHg + CVP, severe tricuspid regurgitation, decreased right ventricular function (as assessed by a Tricuspid annular plane systolic excursion of 10 mm) and flattened septum, suggestive of right ventricular overload (Figure 4). A right heart catheterization was performed revealing pulmonary pressures of 105/45 mmHg with a mean of 63 mmHg, a wedge pressure of 11 mmHg, a pulmonary vascular resistance of 13.19 Wood units and a cardiac output of 3.94 L/min.
The patient was admitted to the intensive care unit to start treatment with intravenous treprostinil and was eventually discharged home with subcutaneous treprostrinil.
Pulmonary arterial hypertension (PAH) is a disease of the pulmonary circulation characterized by a progressive elevation in pulmonary vascular resistance that leads to right ventricular failure and premature death. It is defined as a mean pulmonary artery pressure at rest of 25 mmHg or higher (1). Idiopathic (group 1) PAH requires the exclusion of parenchymal pathology or venous thromboembolic disease as well as a mean wedge pressure less than 15 mmHg. The initial symptoms of PH are the result of an inability to adequately increase cardiac output during exercise which eventually will progress to signs and symptoms of right ventricular failure such as lower extremity edema, syncope/presyncope and chest pain (2,3). Early recognition is of paramount importance to institute adequate treatment.
Roberto J. Bernardo, MD and Carlos Tafich Rios, MD
Internal Medicine Residency, Department of Medicine
University of Arizona, Tucson, AZ
References
- McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College. Circulation. 2009. 119:2250-94. [CrossRef] [PubMed]
- Runo JR, Loyd JE. Primary pulmonary hypertension. Lancet. 2003. 361:1533-44. [CrossRef] [PubMed]
- Peacock AJ. Primary pulmonary hypertension. Thorax. 1999;54:1107-18. [CrossRef] [PubMed]
Reference as: Bernardo RJ, Rios CT. Medical image of the week: idiopathic pulmonary artery hypertension. Southwest J Pulm Crit Care. 2014;9(2):101-3. doi: http://dx.doi.org/10.13175/swjpcc101-14 PDF