October 2014 Imaging Case of the Month
 Friday, October 3, 2014 at 8:00AM
Friday, October 3, 2014 at 8:00AM Sameh Sakla, M.D.
Clinton Jokerst, M.D.
Department of Medical Imaging
University of Arizona Medical Center
Tucson, AZ
A 53-year-old man presents with fatigue and dyspnea on exertion. An admission chest radiograph (Figure 1) was obtained.
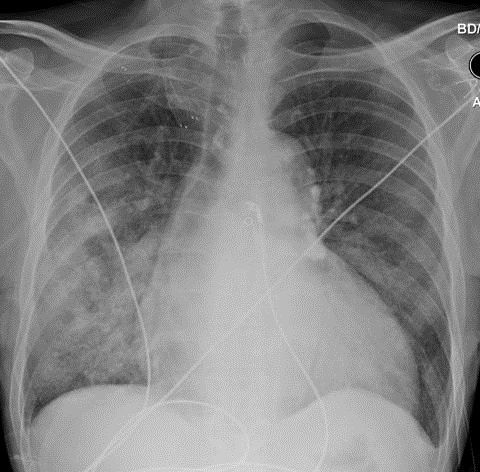
Figure 1. Admission chest radiograph.
What is the best term or phrase used to describe the salient radiographic abnormality?
- Diffuse thick-walled cavitary lesions
- Interstitial and alveolar pulmonary edema with effusions
- Miliary nodules
- Patchy consolidation
- Tension pneumothorax
Reference as: Sakla S, Jokerst C. October 2014 imaging case of the month. Southwest J Pulm Crit Care. 2014;9(4):214-8. doi: http://dx.doi.org/10.13175/swjpcc126-14 PDF


