Medical Image of the Week: NG Tube Misplacement with a Pneumothorax
 Wednesday, January 4, 2017 at 8:00AM
Wednesday, January 4, 2017 at 8:00AM 
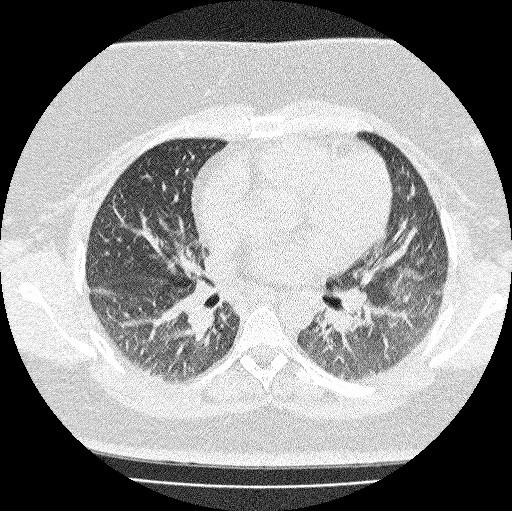
Figure 1. CXR AP view showing misplaced NG tube in the right lung with small pneumothorax.

Figure 2. Follow up CXR AP view showing enlarged right pneumothorax after withdrawal of the NG tube.

Figure 3. CXR AP view post chest tube placement showing reinflation of the right lung.
Nasogastric tube (NG) placement is a common procedure performed in the inpatient hospital setting. They are often challenging to insert and therefore carry a risk of tracheobronchopleural, intravascular and enteral complications.
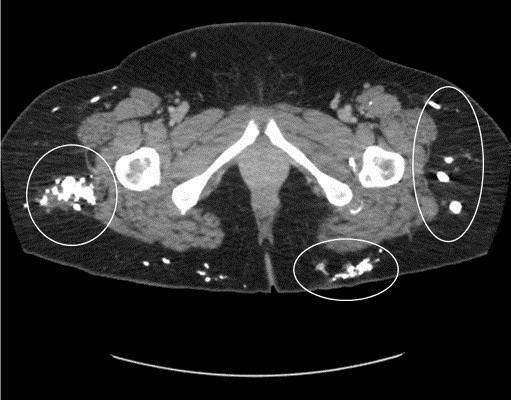
Our patient is a 90-year-old man who was admitted to the hospital with complaints of productive cough, fever, worsening of shortness of breath and confusion. He was diagnosed with viral upper respiratory tract infection, Legionella pneumonia and exacerbation of heart failure. Throughout his hospitalization patient had repeated episodes of delirium and had failed a swallowing evaluation. A NG was inserted for administration of enteral feeds and medications. There was no resistance to the passage of the tube when initially placed. However, post procedure CXR showed a misplaced nasogastric tube going into the right main bronchus and down into right lower lobe with a small apical pneumothorax (Figure 1). Follow up chest X-ray two hours later showed enlargement of the pneumothorax (Figure 2). A 14 Fr pigtail catheter was promptly inserted in right pleural space. A repeat chest X-ray confirmed placement of the chest tube and showed re-inflation of the lung (Figure 3).
The reported incidence of misplacement of nasogastric tubes into the airways ranges from 0.3% to 15% and is more common after chest trauma or mechanical ventilation (1). This may be because of the need for adequate coordination of swallowing. Nasogastric tubes are generally considered safe, but there is a risk of significant pulmonary complications from blind insertion of small-caliber nasogastric tubes with a stiff stylet, particularly in elderly patients with altered mental status as well as with poor swallowing function (2).
Santhosh G. John MD, Vivian Keenan MD, Naveen Tyagi MD, and Priya Agarwala MD
Division of Pulmonary and Critical Care Medicine
Winthrop University Hospital
Mineola, New York USA
References
- Agha R, Siddiqui MR. Pneumothorax after nasogastric tube insertion. JRSM Short Rep. 2011 Apr 6;2(4):28. [CrossRef] [PubMed]
- Nazir T, Punekar S. Images in clinical medicine. Pneumothorax--an uncommon complication of a common procedure. N Engl J Med. 2010 Jul 29;363(5):462. [CrossRef] [PubMed]
Cite as: John SG, Keenan V, Tyagi N, Agarwala P. Medical image of the week: NG tube misplacement with a pneumothorax. Southwest J Pulm Crit Care. 2017:14(1):14-5. doi: https://dx.doi/10.13175/swjpcc133-16 PDF