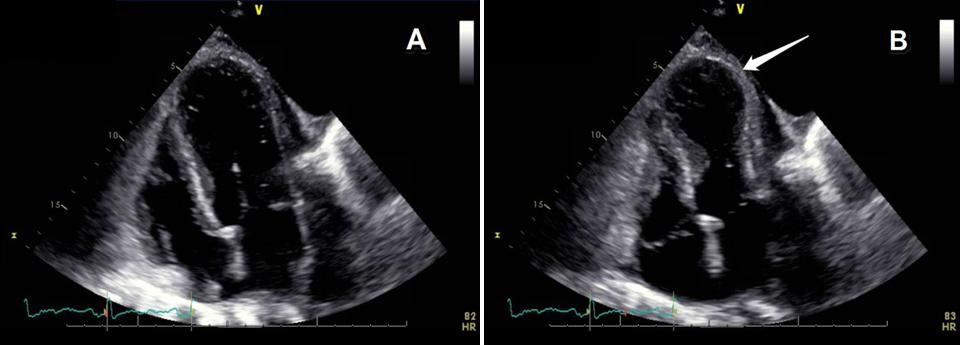
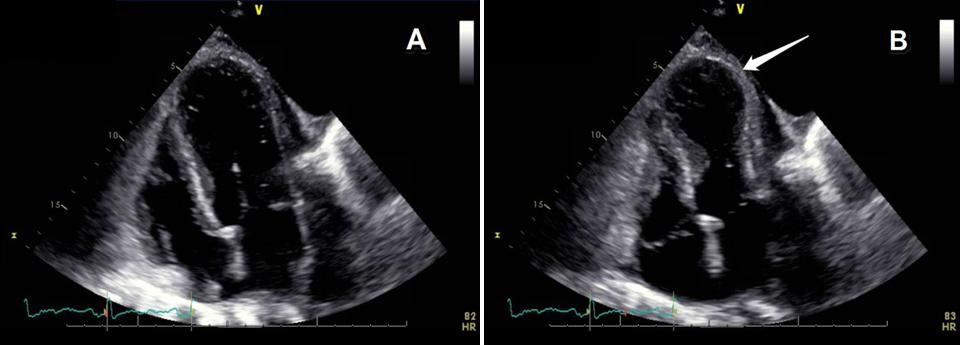
 Figure 1. Panel A: Four chamber view of the heart at the end of diastole with a dilated left ventricle. Panel B: Same four chamber view of the heart at the end of systole with a dilation and akinesis of the apical portion (arrow) of the heart consistent with apical ballooning/stress cardiomyopathy
Figure 1. Panel A: Four chamber view of the heart at the end of diastole with a dilated left ventricle. Panel B: Same four chamber view of the heart at the end of systole with a dilation and akinesis of the apical portion (arrow) of the heart consistent with apical ballooning/stress cardiomyopathy
A 79 year old man with a history of lung cancer. bladder cancer, chronic obstructive pulmonary disease, and coronary artery disease with two previous myocardial infarctions, presented to the emergency department with respiratory failure secondary to pulmonary edema. Further evaluation was significant for non-ST segment elevation myocardial infarction. Cardiac catheterization was remarkable for a focal, eccentric 95% stenosis of the proximal to mid left anterior descending artery that failed stenting due to extensive calcifications. An echocardiogram (ECHO, Figure 1) revealed an ejection fraction of 47% with akinesis of the mid to distal anterior, lateral, inferior, septal and apical segments consistent with takotsubo cardiomyopathy.
Takotsubo cardiomyopathy, aka apical ballooning syndrome or stress induced cardiomyopathy, is a subtype of heart failure typically defined by proposed criteria from the Mayo Clinic that includes: 1. transient hypokinesis, akinesis, or dyskinesis in the left ventricular mid segments with or without apical involvement frequently occurring, but not always, in context to a stressful trigger; 2. the absence of angiographic evidence of obstructive coronary disease or plaque rupture; 3. new ECG abnormalities (ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin; and 4. the absence of pheochromocytoma and myocarditis (1). It predominantly occurs in post-menopausal women in relation to unexpected emotional or physical stress. Characteristic ECHO findings demonstrate a symmetrical regional wall motion abnormalities extending equally into the apical inferior and lateral wall with overall global hypokinesia (Figure 1) (2).
Sachin Kalarn MSIV; Sophie Galson MD; Kristina Skinner DO; Ryan Nahapetian MD, MPH
University of Arizona
Tucson, AZ
References
-
Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118(25):2754-62.
[CrossRef] [PubMed]
-
Chockalingam A, Xie GY, Dellsperger KC. Echocardiography in stress cardiomyopathy and acute LVOT obstruction. Int J Cardiovasc Imaging. 2010;26(5):527-35.
[CrossRef] [PubMed]
Reference as: Kalarn S, Galson S, Skinner K, Nahapetian R. Medical image of the week: ECHO findings of aprical ballooning syndrome. Southwest J Pulm Crit Care. 2015;10(4):150-1. doi: http://dx.doi.org/10.13175/swjpcc024-15 PDF
 Friday, April 3, 2015 at 8:00AM
Friday, April 3, 2015 at 8:00AM