Leadership in Action: A Student-Run Designated Emphasis in Healthcare Leadership
 Friday, March 25, 2022 at 8:00AM
Friday, March 25, 2022 at 8:00AM Morcel Hamidy, BS1
Kishan Patel, BS1
Sonul Gupta, BS1,
Manparbodh Kaur, BS1
Jordan Smith, MD2
Haeli Gutierrez, BS1
Mohamed El-Farra, MS1
Natalie Albasha, BS MS1
Priya Rajan, BA1
Secilia Salem, BS1
Somiya Maheshwari, BS1
Kendrick Davis, PhD3
Brigham C Willis, MD, MEd4
1Medical Student, UC Riverside School of Medicine
2Resident, Loma Linda Pediatric Residency Program
3Associate Dean of Assessment and Evaluation, UC Riverside School of Medicine
4Senior Associate Dean of Medical Education, UC Riverside School of Medicine
Abstract
Background: Throughout medical school students are exposed to a variety of fields within medicine, but structured leadership and teaching opportunities are limited. There is a need for more training to prepare students of all backgrounds to be future leaders in all healthcare realms, especially critical care medicine, in order to address the lack of diversity seen in leadership positions.
Methods: Implemented entirely by students with faculty guidance, the Kern model was applied to develop a student-run longitudinal Designated Emphasis in Healthcare Leadership. This program was implemented at a medical school leading the nation in creating opportunities for diverse and underrepresented groups in medicine. Students are involved in structured leadership lectures, projects, and mentorship, and there is an emphasis on learning by doing. A survey was sent out to all present and past student participants to assess its acceptability and effectiveness.
Results: A post-participation survey found that a total of 96% of participants identified themselves as healthcare leaders, felt confident leading a team, and felt comfortable working with a diverse team. Further, 96% of participants agreed or strongly agreed they would recommend the program to other medical students. Qualitative feedback revealed that participants felt they learned how to “apply leadership skills to the healthcare setting” and were provided an “environment to grow and practice vital leadership skills that will help [them] be effective clinicians.”
Conclusions: Our initial research shows that introducing a longitudinal leadership program into Medical Education may allow participants to start developing personal and professional leadership qualities. The program is well-received by the students and preliminary data shows that there may be increase in leadership capabilities when participating in this program. Such a program can enable future healthcare providers to become leaders in their own fields, so that they can hone interpersonal communication skills, bridge the gap of representation in leadership positions, and lead teams effectively.
Introduction
Responding to critical care emergencies requires effective coordination and management of multiple healthcare providers. Hence, leadership skills and multidisciplinary teamwork are recognized as significant curricular milestones and learning objectives for pulmonary and critical care medicine (PCCM) learners by the Accreditation Council for Graduate Medical Education (ACGME) (1). Effective communication and leadership acumen are critical non-medical aspects of successful patient management in the intensive care unit (ICU), often leading to increased performance and improve patient outcomes (2,3). Despite this, leadership training opportunities are variable from program to program, with no clear consensus on the components of effective leadership curricula. As a result, there are no guidelines on a standardized leadership curricula in critical care medicine or undergraduate medical education (4,5).
There has been some progress within the undergraduate medical education community to integrate healthcare leadership into medical curricula. The number of MD-MBA dual degree programs grew by 25% from 2011 to 2012 alone (6). However, only a fraction of medical schools provide students with opportunities for medical leadership training, with courses typically being elective (7). The Association of American Medical Colleges (AAMC) stated that graduating medical students should learn “leadership skills that enhance team functioning, the learning environment, and/or the health care delivery system” (8). In 2015, a survey showed that 46 out of 88 allopathic medical schools had some form of leadership curriculum.7,9 The curricula of these schools included: mentoring programs (65.1%), dual degree programs (54.5%), workshops (48.8%), seminar/lecture series (41.9%), courses (41.9%), or single seminars (18.6%). However, despite the rise in importance of leadership education, only 19% percent of those institutions offered a longitudinal leadership education throughout medical school (9).
There is also a need to address inequities in healthcare leadership. A recent AAMC report on diversity and inclusion in Medical School Deans found that only 11% of US Medical School Deans are underrepresented in medicine (URiM). Further, the report highlighted that this number has been stagnant over the past 30 years, growing from 7% in 1991 to only 11% in 2020 - an alarming trend highlighting the barriers to ensuring appropriate representation in our healthcare leadership positions (10). The UC Riverside School of Medicine (UCR SOM) has been at the forefront of bridging the gaps in inequities. It was recently named the sixth most diverse medical school in the nation based on metrics of student enrollment of underrepresented in medicine background, percent of graduates practicing in primary care and rural medicine, and percent of graduates eventually working in underserved regions (US News). The UCR SOM led these metrics with an outstanding 34.1% student population from underrepresented in medicine backgrounds. Hence, programs led at the UCR SOM reflect a growing trend attempting to bridge gaps in leadership representation (11).
To address these needs, we created a student-run leadership program using the Kern Six-Step Model highlighting competencies considered fundamental to leadership development (12). The goal was to develop longitudinal leadership training at the undergraduate medical education level to train future providers to have confidence and readiness to manage interdisciplinary teams in complex medical situations, such as the ICU. As a student-run program with support of faculty, we report a detailed description of the Healthcare Leadership Program (HLP) in the hopes that it may be helpful to implement a standardized leadership training model at other institutions.
Methods
To implement the Healthcare Leadership Program (HLP) as a Designated Emphasis within Medical Education, students met with a faculty mentor to establish topics and activities (Appendix A and Appendix B) that met credit requirements set by the School of Medicine. A leadership structure (Appendix C) that focused on student oversight was then established. In addition to the lecture and workshop curriculum, students were expected to actively participate in mentorship and projects. This amounted to a total of 30 units distributed across the four-year program, allowing for 320 contact hours with 304 required hours to obtain a Designated Emphasis in Healthcare Leadership. Upon completion, students are given a distinction on their Medical Student Performance Evaluation (MSPE) and their diplomas. Selection of students was done through an application (Appendix D) and interview process.
Special attention was taken to accept students from a variety of diverse backgrounds in order to help bridge inequities currently seen in healthcare leadership. This was done through an interviewing process and holistic review of applicants. The number of students increased annually as the program grew stronger and obtained more resources. The initial cohort started with 8 total students throughout all medical school years, and currently the number of students per year is capped at 10 students per year due to restraints in educational resources available. The current attrition rate is 4% of students deciding to not continue with the program.
For the first-year curriculum (Appendix A), students were expected to complete a minimum of 14 hours. The aim of the year was to build a strong leadership foundation by teaching leadership fundamentals, helping students understand their own strengths, and how to effectively collaborate with peers. Activities included students learning about their own strengths and weaknesses through a formalized StrengthsFinder assessment. Students were also taught to improve efficiency and reduce waste in organizations through LEAN/6 Sigma White and Yellow Belt training. Further, guest speakers supplemented learning by teaching topics including communication skills, leading meetings, conflict resolution, and networking. A full list of topics taught during the 2018-2019 academic year are included in Appendix A.
For the second-year curriculum (Appendix B), students were expected to complete a minimum of 10 hours. During the second-year, we focused on growing students into healthcare leaders. The curriculum focused on healthcare leadership and medical management by teaching the most common and relevant principles from Masters in Business Administration (MBA), Masters in Public Policy (MPP), and Masters in Public Health (MPH) programs. The goals and objectives for the students were taught through mixed media including online lectures, lecturer workshops, and discussions with community leaders. A full list of topics taught during the 2019-2020 academic year are included in Appendix B.
For the third and fourth-year curriculum, the focus was to have student leaders practice what they learned in the first two years and apply it to the professional world. For the third and fourth year, students engage in selectives. Selectives are 3 weeks during the third year totaling 12 units for 120 hours and 4 weeks during the fourth year totaling 16 units for 160 hours. The selective was comprised of five different parts including hands-on experience in a clinical setting, observation of current practices, formal report of possible improvements, resource summaries, and continued participation in mentorship programs. Selectives are self-created by HLP students, with the help of HLP board members and faculty advisors. Third and fourth-year students were assessed via a form included in Appendix E.
It is important to note that in this student-run program, the students themselves were responsible for coordinating and executing the lectures. The majority of lectures were given by students from previous cohorts, and this cycle continued where each cohort was responsible for educating the following cohort. Occasionally, guest lecturers were asked to come and teach the students. The material was saved and uploaded to an online drive for the following years to be able to access in order to maintain fidelity of the curriculum.
Outside of the structured curriculum, each student is required to work on a project of their choice in the first two years of medical school. The goal of this requirement is to allow student leaders to gain experience in navigating bureaucracies, innovation, and building teamwork and networking skills through hands-on experience on a topic they feel passionate about. Students pay special attention to initial measurements to identify baseline data, implementation of intervention, and collecting results, with an ultimate goal of publishing the project. At the end of the project, students make a formal presentation to the HLP Board and School of Medicine Leadership.
This project also prepares students for their fourth-year capstone projects. During this time students have the opportunity to spend four weeks at a clinical site, observing current operating procedures in an effort to identify strengths that they can employ in their future practice, and weaknesses that could be improved. Students are assigned a faculty advisor and are responsible for designing one intervention aimed at improving efficiency and reducing waste, based on their observations. After incorporating feedback, students have the opportunity to implement their proposed project at the site.
HLP is made up of general members and executive board members, all exclusively students. Appendix C highlights the structure of the executive board which is made up of three tiers. The first tier includes the Member Development Officer, Operations Officer, Medical Education Officer, and Community Relations Officer who are primarily responsible for first year HLP general members. The second tier consists of the Chief Innovation Officer, Chief Operations Manager, Chief Medical Education Officer, and Chief Community Relations Officer and are responsible for the second year HLP students in addition to managing the officers in tier one. In tier three, the Chief Executive Officer oversees the rest of the officer board and manages communication with the School of Medicine Leadership and administration. Finally, the HLP Alumni Advisory Board is a network of graduated HLP medical students who offer guidance and support to the executive board. The specific responsibilities of the executive board positions can be found in Appendix C.
In addition to lectures and workshops, students are expected to participate in formal mentorship. Mentorship pairing occurred in the first year, after students shared a biography of their past experiences, interests, and passions. The Community Relations Officers met with each individual student to discuss their interests and career aspirations. The Officer then works with the rest of the Executive Board and Advisors in helping place students with the right mentor. Students in the program are connected with local CEO’s, CMO’s, Dean’s, Business Specialists, and Residency Program Directors. The mentor-mentee relationship is cultivated over the duration of the medical student’s training, as the students finalize their career path and passion projects.
Aligning with Kern Model Step 6: Evaluation and Feedback (12), surveys were sent out periodically to evaluate the effectiveness of the curriculum. A survey was sent out regarding all first-year lectures which was completed by the entire cohort (Appendix F). Results of this survey helped plan the first-year lectures for the next cohort. A survey was also sent out to assess the effectiveness of the program as a whole, which was completed by the entire HLP Cohort (Appendix G). The Institutional Review Board (IRB) did not review our project as it was conducted for the purposes of course improvement and evaluation, and therefore, IRB review was not required.
Results
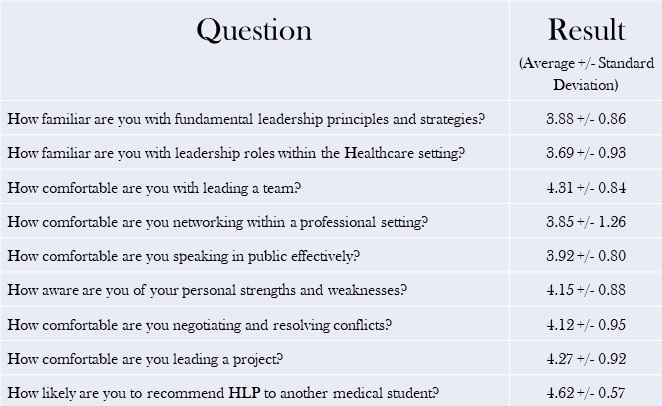
The program was implemented with a total cohort of 25 participants. A post-participation survey (Appendix G) was sent to participants to understand their personal growth and learning throughout the program. Participant responses to various questions detailing their healthcare leadership education through HLP was noted using a questionnaire using a 1 through 5 scale, with 1 indicating very low, 2 indicating low, 3 indicating neutral, 4 indicating high, and 5 indicating very highly. Results are shown in Table 1.
Table 1. Participant questionnaire responses to various questions detailing their healthcare leadership education through HLP was noted using a questionnaire using a 1 through 5 scale, with 1 indicating very low, 2 indicating low, 3 indicating neutral, 4 indicating high, and 5 indicating very highly. The entire cohort of 25 students was surveyed.
Participants were also asked to note if they strongly disagree, disagree, neutral, agree, or strongly agree with statements reflecting on their personal capabilities as a leader. Results are included in Figure 1.
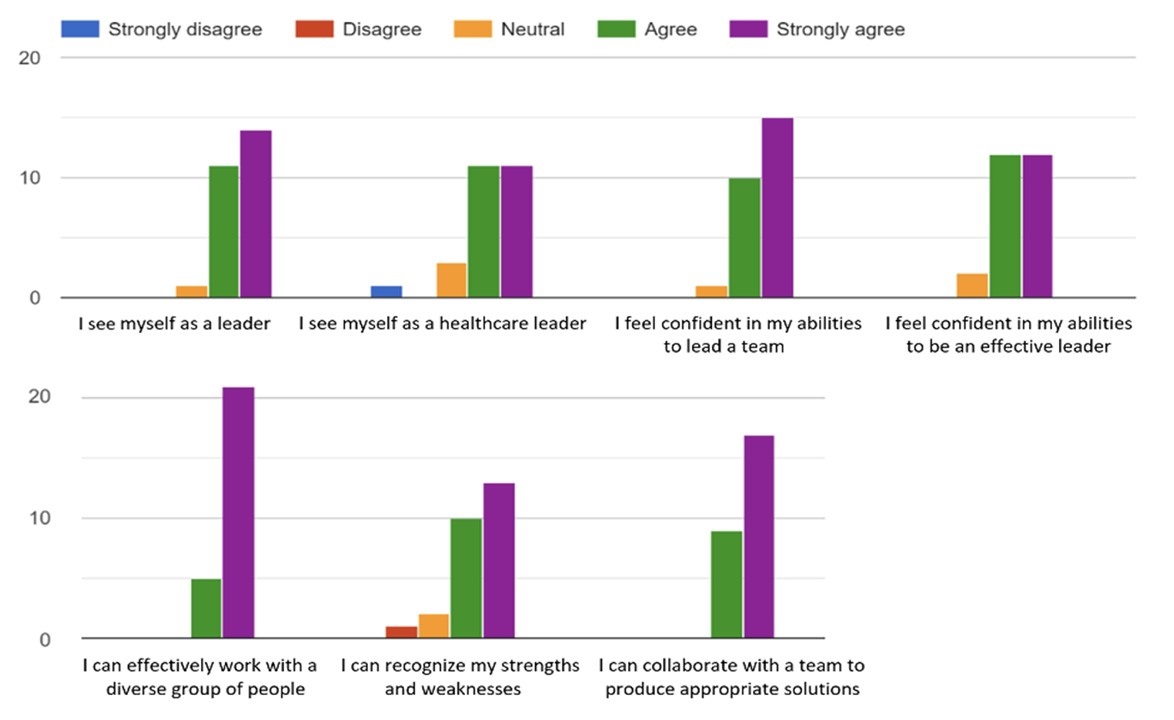
Figure 1. Results for the question “how strongly do you agree with the following statements” pertaining to personal leadership capabilities. The entire cohort of 25 students was surveyed. The y-axis represents the number of students that agree with the above statements.
All 25 students of the cohort were surveyed for this data collection.
A total of 96% of participants agreed or strongly agreed that they identified themselves as a healthcare leader, felt confident leading a team, and felt comfortable working with a diverse team. Further, 96% of participants agreed or strongly agreed they would recommend the program to other medical students.
Students were given the opportunity to share comments throughout the survey. Participants felt they learned how to “apply leadership skills to the healthcare setting” and were provided an “environment to grow and practice vital leadership skills that will help [them] be effective clinicians.” Other comments highlight community building within HLP, such as “I have been able to meet people who are very much like-minded. That in itself is very nourishing.” Anecdotal evidence also suggests that students value HLP’s curriculum as it “prepares students for professional goals” and allows for “hands-on experience in grant writing and research.”
A prevailing theme among participants was that students enjoyed the autonomy of the program to explore their interests and passions. Students stated that, “Individuals lead in different manners and to only provide one cookie-cutter set of leadership instruction would be limiting to the diverse members of HLP” and that they enjoy the “flexibility to pursue anything [they] want under the large umbrella of leadership.”
However, with this flexibility and fluidity of the program, came some critiques as well. One student noted that, “The curriculum seems scattered to me … while it is good to learn a diversity of information, a lack of direction leaves the curriculum feeling disorganized.” Another recommendation was the desire for more networking opportunities with faculty and other students: “A lot of our speakers are Faculty, and I think we can learn some new perspectives and tools if we branch beyond our networks.” The current model of HLP was that the second, third, and fourth-year medical students help network to find mentors for the first-year students. Some students noted that perhaps we should, “encourage the first years to do so by hosting a seminar-like session where we could encourage networking [because] by doing it for them, we are limiting their own involvement and learning.”
The results of the Healthcare Leadership Program were also measured by the success of the projects that have started within the program. The dual nature of students being facilitators as well as learners was unique to HLP, as students played an active role in their education. Hands-on experience was integral and allowed students to participate in passion-driven specific ventures.
For example, members of HLP participated in a Quality Improvement project at a Student-Run Free Clinic. After first observing the clinic flow, HLP members came together to brainstorm ways to optimize clinic efficiency and proposed a number of interventions. The team then presented changes to the Board of the Free Clinic, received approval, and implemented the interventions. This project improved the workflow and optimized efficiency of the Free Clinic, resulting in a statistically significant decrease in patient door-to-door times. Students then published this data at the American Medical Association Research Symposium December 2020 (Appendix H).
Discussion
Many demanding specialties, particularly PCCM, require extensive leadership skills. Despite this, most medical schools lack any formal, longitudinal leadership training integrated into the curriculum9. One possible reason for the lack of leadership curricula may be that there is a lack of consensus on what leadership competencies should be emphasized (13,14). Many have proposed a curriculum that focuses on emotional intelligence, self-reflection, and communication skills to be among the most effective (13,15,16,17). Our program encourages these skills via lectures as well as hands-on projects where they put leadership skills learned into practice in interdisciplinary clinical settings. Our program is focused on drawing out the passions and interests possessed by medical students, and teaching them to sharpen their leadership skills to be effective leaders. HLP is focused on a “learning-by-doing” model (17), where students are first equipped with the tools, they need to be effective and then allowed to practice these skills in projects they care about.
HLP is an innovative Designated Emphasis that has been ongoing for four years. As a student led organization, the development has been flexible and adaptable to student needs and interests, with guidance by appropriate mentors for different topics. Our preliminary data shows HLP to be well received by the current cohort, in which 96% of students identified themselves as a healthcare leader. Further, 96% of participants agreed or strongly agreed they would recommend the program to other medical students. HLP is a dynamic, ever-changing program, where we utilize the innate skills and passions of use students to constantly reshape the curricula to fit the needs of the students in that cohort. Feedback is encouraged in every step of the program, as all students share the growth-mindset ideology of utilizing feedback to better the program.
As a new, developing program, HLP has some limitations. The program covers the most common leadership positions, but it does not cover all possible avenues of leadership, and some of the more unique positions may not be explored as in depth. Another limitation is that due to current resources, only a limited number of applicants can be accepted into the Designated Emphasis. In particular, one of the most limiting resources is available and engaged mentors. A strong and significant network of physician leaders is imperative for the program’s success.
It is our hope that HLP can be used as a template and be incorporated into the medical education curriculum at other schools as a Designated Emphasis, Selective, Thread, or Interest Group. The organized curriculum can be used as a guided lecture series throughout medical school but can also be utilized in PCCM residency programs. The program gives great exposure to what different leadership programs may look like, including Master’s and other graduate programs, and can be used as a guide for medical students and residents to focus their interests. Additionally, the HLP will create opportunities for building strong leadership skills early on that can help prepare future PCCM physicians of tomorrow.
Acknowledgements
We would like to acknowledge the founders of the Healthcare Leadership Program at UC Riverside School of Medicine: Matt Gomez MD, Nekisa Haghighat MD, MPH, Frances Tao MD, MPH, and Cassidy Lee MS, MPP, along with the help of their faculty advisor, Paul Lyons MD. We would also like to thank Ms. Elisa Cortez for her help with literature review.
References
- Fessler HE, Addrizzo-Harris D, Beck JM, Buckley JD, Pastores SM, Piquette CA, Rowley JA, Spevetz A. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: report of a multisociety working group. Chest. 2014 Sep;146(3):813-834. [CrossRef] [PubMed]
- Schmutz J, Manser T. Do team processes really have an effect on clinical performance? A systematic literature review. Br J Anaesth. 2013 Apr;110(4):529-44. [CrossRef] [PubMed]
- Hunziker S, Johansson AC, Tschan F, Semmer NK, Rock L, Howell MD, Marsch S. Teamwork and leadership in cardiopulmonary resuscitation. J Am Coll Cardiol. 2011 Jun 14;57(24):2381-8. [CrossRef] [PubMed]
- Clyne B, Rapoza B, George P. Leadership in Undergraduate Medical Education: Training Future Physician Leaders. R I Med J (2013). 2015 Sep 1;98(9):36-40. [PubMed]
- Rosenman ED, Shandro JR, Ilgen JS, Harper AL, Fernandez R. Leadership training in health care action teams: a systematic review. Acad Med. 2014 Sep;89(9):1295-306. [CrossRef] [PubMed]
- Goyal R, Aung KK, Oh B, Hwang TJ, Besancon E, Jain SH. AM last page. Survey of MD/MBA programs: opportunities for physician management education. Acad Med. 2015 Jan;90(1):121. [CrossRef] [PubMed]
- Neeley SM, Clyne B, Resnick-Ault D. The state of leadership education in US medical schools: results of a national survey. Med Educ Online. 2017;22(1):1301697. [CrossRef] [PubMed]
- AAMC organization. Core entrustable professional activities for entering residency. https://www.aamc.org/system/files/c/2/482194-epa4toolkit.pdf. Accessed October 21, 2021.
- Richard K, Noujaim M, Thorndyke LE, Fischer MA. Preparing Medical Students to Be Physician Leaders: A Leadership Training Program for Students Designed and Led by Students. MedEdPORTAL. 2019 Dec 13;15:10863. [CrossRef] [PubMed]
- U.S. medical school deans by Dean type And Race/ethnicity (URIM vs. non-URiM). AAMC. https://www.aamc.org/data-reports/faculty-institutions/interactive-data/us-medical-school-deans-trends-type-and-race-ethnicity (accessed March 21, 2022)..
- Morse R, Castonguay A, Vega-Rodriguez, J, Brooks E, Hines K. Most Diverse Medical Schools. https://www.usnews.com/best-graduate-schools/top-medical-schools/medical-school-diversity-rankings. Published March 30, 2020 (accessed March 21, 2022).
- Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach. Baltimore, MD: Johns Hopkins University Press;2015:1-300.
- Stoller JK. Developing physician-leaders: a call to action. J Gen Intern Med. 2009 Jul;24(7):876-8. [CrossRef] [PubMed]
- Lobas JG. Leadership in academic medicine: capabilities and conditions for organizational success. Am J Med. 2006 Jul;119(7):617-21. [CrossRef] [PubMed]
- Stoller JK. Developing physician-leaders: key competencies and available programs. J Health Adm Educ. 2008 Fall;25(4):307-28. [PubMed]
- Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ. 2014 Mar;6(1):21-31. [CrossRef] [PubMed]
- Reese, H. W. (2011). The learning-by-doing principle. Behavioral Development Bulletin. 2011;17(1):1-19. [CrossRef]

Reader Comments