Results of the SWJPCC Telemedicine Questionnaire
 Wednesday, September 30, 2020 at 8:41AM
Wednesday, September 30, 2020 at 8:41AM Richard A. Robbins, MD
Julene R. Robbins, PhD, NCSP
Phoenix Pulmonary and Critical Care Research and Education Foundation
Gilbert, AZ USA
Abstract
As the COVID-19 crisis puts pressure on outpatient providers to facilitate remote care, some have set aside their skepticism and opened telemedicine clinics as an alternative to the traditional office visit. In these visits, the provider and patient usually are able to visually and verbally interact. However, interactions that require contact such as a physical examination are not possible. We conducted a voluntary, anonymous, on-line survey of the Southwest Journal of Pulmonary and Critical Care (SWJPCC) readership to determine their experience and attitudes toward telemedicine. Of the 84 respondents we surveyed, most were favorable towards telemedicine visits with two-thirds of respondents being very or mostly satisfied with telemedicine. However, some (30%) estimated that over 50% of their time was spent with documentation and a significant portion (55%) noted reduced reimbursement. These data support the Center for Medicare and Medicaid’s (CMS) decision to expand telemedicine beyond the present COVID-19 pandemic.
Introduction
The COVID-19 pandemic has created new challenges for patient care. The risk for severe illness from COVID-19 increases with age (1). Many patients and some providers are elderly and at risk for more severe disease. According to the Centers for Disease Control and Prevention (CDC), the best protection is to limit interactions with other people as much as possible (1).
One potential solution which avoids contraction of COVID-19 by face-to-face exposure is telemedicine. Telemedicine is the remote diagnosis and treatment of patients by means of telecommunications technology usually employing both visual and audio interaction. Telemedicine has been around for some time and its use has increasing (2). However, telemedicine is not without limitations including the obvious concerns of reimbursement, regulatory issues, privacy, the need for access to telemedicine devices (e.g., smartphone, tablet, computer), comfort levels with the technology by both healthcare providers and patients, and cultural acceptance of conducting virtual visits in lieu of in-person visits (3). Furthermore, other fundamental issues such as selection of patients and outcomes are largely unknown.
To discover the experiences with and the attitudes toward telemedicine, we posted an on-line questionnaire and solicited the Southwest Journal of Pulmonary and Critical Care (SWJPCC) readership to fill out the questionnaire The results suggest that telemedicine usage has increased with the COVID-19 pandemic, and despite the short time of implementation, is generally acceptable to providers.
Methods
Questionnaire
A questionnaire was constructed with the goals of determining healthcare providers experience and attitudes towards telemedicine. An additional goal was to keep the survey brief, since previous experience was that long surveys usually have a poor response. A series of 11 questions was developed (Appendix 1).
Data Collection and Statistical Analysis
Data was collected August 9, 2020 through August 31, 2020. The data was collected on the Southwest Journal of Pulmonary and Critical Care website using Excel.
Results
Demographics
There were 84 respondents. Eighty-one answered yes to offering telemedicine but 3 no’s appeared to have prior experience with telemedicine (Appendix 2). Although we did not question which were physicians, nurse practitioners, physician assistants, etc., the vast majority of respondents to previous SWJPCC surveys have been pulmonary and critical care physicians (4).
Sixty-eight of the eighty-four respondents (81%) did not offer telemedicine before the COVID-19 pandemic. The majority of these 64/84 (76%) offered telemedicine to both new and established patients. Only 20/84 (24%) offered telemedicine to established patients only.
Telemedicine platform
There were 90 responses from the 84 respondents to which telemedicine platform was being used. Some respondents apparently used more than one platform.
Table 1. Telemedicine platforms used.
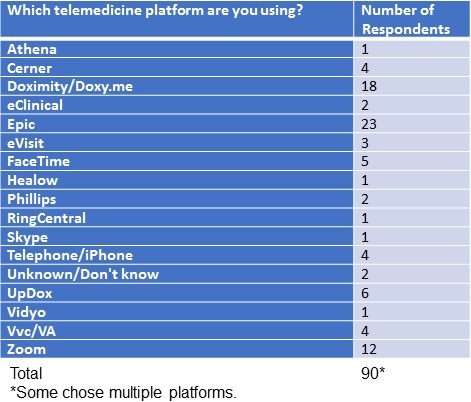
The most common reason cited for using a platform was that the telemedicine platform was offered with the electronic healthcare record currently in use (30 of 84, 36%). An almost an equal number (29/84, 35%) did not know the basis of choosing the platform and presumably had not been involved in the selection process. Only 4 said the platform was chosen on the basis of reviews.
Connectivity
A major concern of telemedicine has been the ability of some patients and providers to use the technology (3). This would likely be reflected in a low number of patients and providers to establish a connection. The results of the questionnaire suggest connectivity is not a major problem (Figure 1).
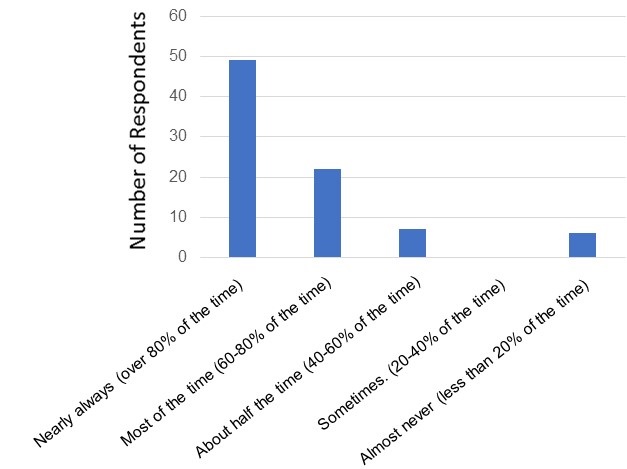
Figure 1. Connectivity of telemedicine visits. Number of respondents is on the vertical axis and their responses are on the horizontal axis.
There was no consistent pattern in those who had problems with connections (Appendix 2).
Satisfaction
Two-thirds of the respondents were either very or mostly satisfied with their current telemedicine platform (Figure 2).
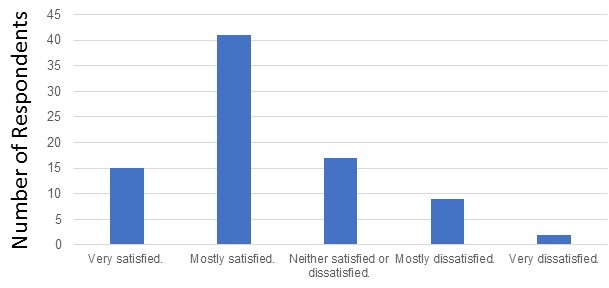
Figure 2. Satisfaction with current telemedicine system.
There was no consistent pattern to telemedicine satisfaction although other than only one of the seven respondents who used eVisit (Banner Healthcare system) or the VA system was satisfied (Appendix 3).
Disadvantages of Telemedicine
The five most common disadvantages of telemedicine as viewed by the respondents are listed in Table 2.
Table 2. Most common disadvantages of telemedicine.
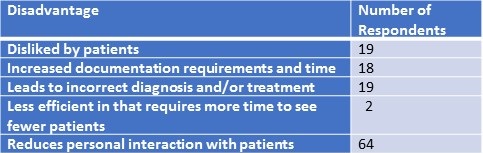
No other pattern of responses was discerned other than four noting the obvious lack of vitals and physical exams possible with telemedicine. The questionnaire also asked specifically about time for documentation and reimbursement because one of the authors (RAR) noted high documentation time and low reimbursement in his practice. Documentation time did tend to be high (Appendix 2). Twenty-five respondents (30%) noted that over half the time of a telemedicine visits was spent in documentation and/or billing. Many respondents (35 out of 84, 42%) did not know the reimbursement for the telemedicine visits compared to a face-to-face office visit. One respondent claimed a higher reimbursement with telemedicine; 21 (25%) claimed reimbursement was about the same; and the remainder (74%) claimed lower reimbursement (Appendix 2).
Advantages of Telemedicine
Some advantages of telemedicine are obvious such as decreased exposure to COVID-19. This was noted by a majority of our respondents (80 out of 84 (95%), Table 3).
Table 3. Advantages of telemedicine.
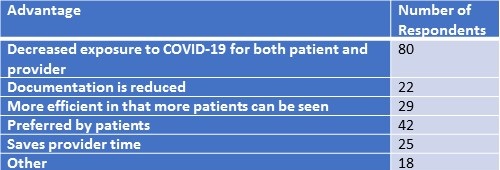
Other advantages cited included patient preference (42 respondents, 50%); more efficient time utilization (29 respondents, 35%); provider time savings (25 respondents, 30%); and reduced documentation (22 respondents, 26%). There were 11 other responses but none listed by more than 2 respondents.
Discussion
To our knowledge this is the first survey of healthcare providers providing telemedicine since the beginning of the COVID-19 pandemic. Although the sample-size of respondents is not large, it is adequate when compared to relatively smaller number of pulmonary and critical care providers in the Southwest United States. Most (67%) were satisfied with telemedicine. However, 30% noted high documentation times and 55% decreased reimbursement.
Our study is consistent with previous observations that patients are mostly satisfied with telemedicine[HD1] . Gustke et al. (5) reported an extraordinarily high patient satisfaction rate of 98.3% from a telemedicine center. Review articles and meta-analysis suggest that telemedicine is acceptable to most patients in a variety of circumstances (6,7). However, many studies have methodological deficiencies such as low sample sizes, context, and study designs which limit generalizability (6,7). Studies clearly defining “when” and “for what” telemedicine should be utilized are needed. Data demonstrating outcomes will be necessary but at the present time such data is lacking.
Telemedicine has been around for some time but has never been fully utilized. In 2019, only 12% of pulmonologists were using telemedicine although its use has slowly been increasing over the past 20 years (7). Telemedicine usage appears to have been markedly accelerated by the COVID-19 pandemic (8). According to The Physicians Foundation’s 2018 Survey of America’s Physicians conducted by Merritt Hawkins, approximately 18% of physicians indicated they were using telemedicine to treat patients in 2018 (9). That number had increased to 48% by April, 2020 according to a new survey (10). In this rush to establish telemedicine if and how much training the providers receive is unclear.
In a survey conducted by American Well physicians several reasons were listed for choosing telemedicine including: 1. Improved patient access to care (93%); 2. More efficient use of time (77%); 3. Reduced healthcare costs (71%); 4. High-quality communications with patients (71%); and 5. Enhanced doctor-patient relationship (60%) (7). Almost certainly contributing to the increase in telemedicine usage has been the relaxation of the Centers for Medicare & Medicaid Services (CMS) rules regarding reimbursement for telemedicine (11). CMS is now proposing changes to expand telemedicine permanently (12).
Telemedicine visits may require less efforts on the part of the support staff. For example, no vitals are needed. No show rates might also improve. Once telemedicine established and up and running, it can also reduce the size of office space required per provider in the clinic. This could help compensate for lower reimbursement by reducing overhead expenses.
It seems likely that telemedicine will persist in some form after the COVID-19 pandemic. What is unclear is which patients should be seen and what reimbursement should be provided. For example, doing an office visit to check on CPAP compliance for a patient with sleep-apnea is probably appropriate and can probably be done efficiently by telemedicine. However, a more complex patient and especially one where a physical examination is important, might require a face-to-face office visit. Further investigation is needed to determine both appropriateness and optimal reimbursement for telemedicine rather than a one telemedicine fits all approach.
References
- Centers for Disease Control and Prevention. Older adults and COVID-19. August 16, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html#:~:text=As%20you%20get%20older%2C%20your,than%20people%20in%20their%2050s. (accessed 9/14/20).
- Health and Human Services. HHS Issues New Report Highlighting Dramatic Trends in Medicare Beneficiary Telehealth Utilization amid COVID-19. July 28. 2020. Available at: https://www.hhs.gov/about/news/2020/07/28/hhs-issues-new-report-highlighting-dramatic-trends-in-medicare-beneficiary-telehealth-utilization-amid-covid-19.html (accessed 9/14/20).
- Centers for Disease Control and Prevention. Using Telehealth to Expand Access to Essential Health Services during the COVID-19 Pandemic. June 10, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html (accessed 9/14/20).
- Robbins RA, Gotway MB, Robbins JR, Wesselius LJ. Results of the SWJPCC healthcare survey. Southwest J Pulm Crit Care. 2020;20(1):9-15. [CrossRef]
- Gustke SS, Balch DC, West VL, Rogers LO. Patient Satisfaction with Telemedicine. Telemedicine Journal. 2004;6(1):5-13. [CrossRef]
- Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320(7248):1517-1520. [CrossRef] [PubMed]
- Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. Published 2017 Aug 3. [CrossRef] [PubMed]
- Zarefsky M. 5 huge ways the pandemic has changed telemedicine. AMA Practice Management. August 26, 2020. Available at: https://www.ama-assn.org/practice-management/digital/5-huge-ways-pandemic-has-changed-telemedicine?gclid=Cj0KCQjwqfz6BRD8ARIsAIXQCf0iteUTWx7lZpFS_uqgkRYc9c4Sjm6iRq9mflmInb-L1H_jvWMszW4aAnsAEALw_wcB (accessed 9/14/20).
- The Physicians Foundation. 2018 Survey of America’s Physicians. Available at: https://physiciansfoundation.org/wp-content/uploads/2018/09/physicians-survey-results-final-2018.pdf (accessed 9/14/20).
- Miliard M. CMS relaxes more rules around telehealth, allowing care across state lines. Healthcare IT News. April 10, 2020. Available at: https://www.healthcareitnews.com/news/cms-relaxes-more-rules-around-telehealth-allowing-care-across-state-lines (accessed 9/14/20).
- Centers for Medicare & Medicaid Services. Trump Administration Proposes to Expand Telehealth Benefits Permanently for Medicare Beneficiaries Beyond the COVID-19 Public Health Emergency and Advances Access to Care in Rural Areas. August 3, 2020. Available at: https://www.cms.gov/newsroom/press-releases/trump-administration-proposes-expand-telehealth-benefits-permanently-medicare-beneficiaries-beyond.
Cite as: Robbins RA, Robbins JR. Results of the SWJPCC Telemedicine Questionnaire. Southwest J Pulm Crit Care. 2020;21:66-72. doi: https://doi.org/10.13175/swjpcc049-20 PDF

Reader Comments